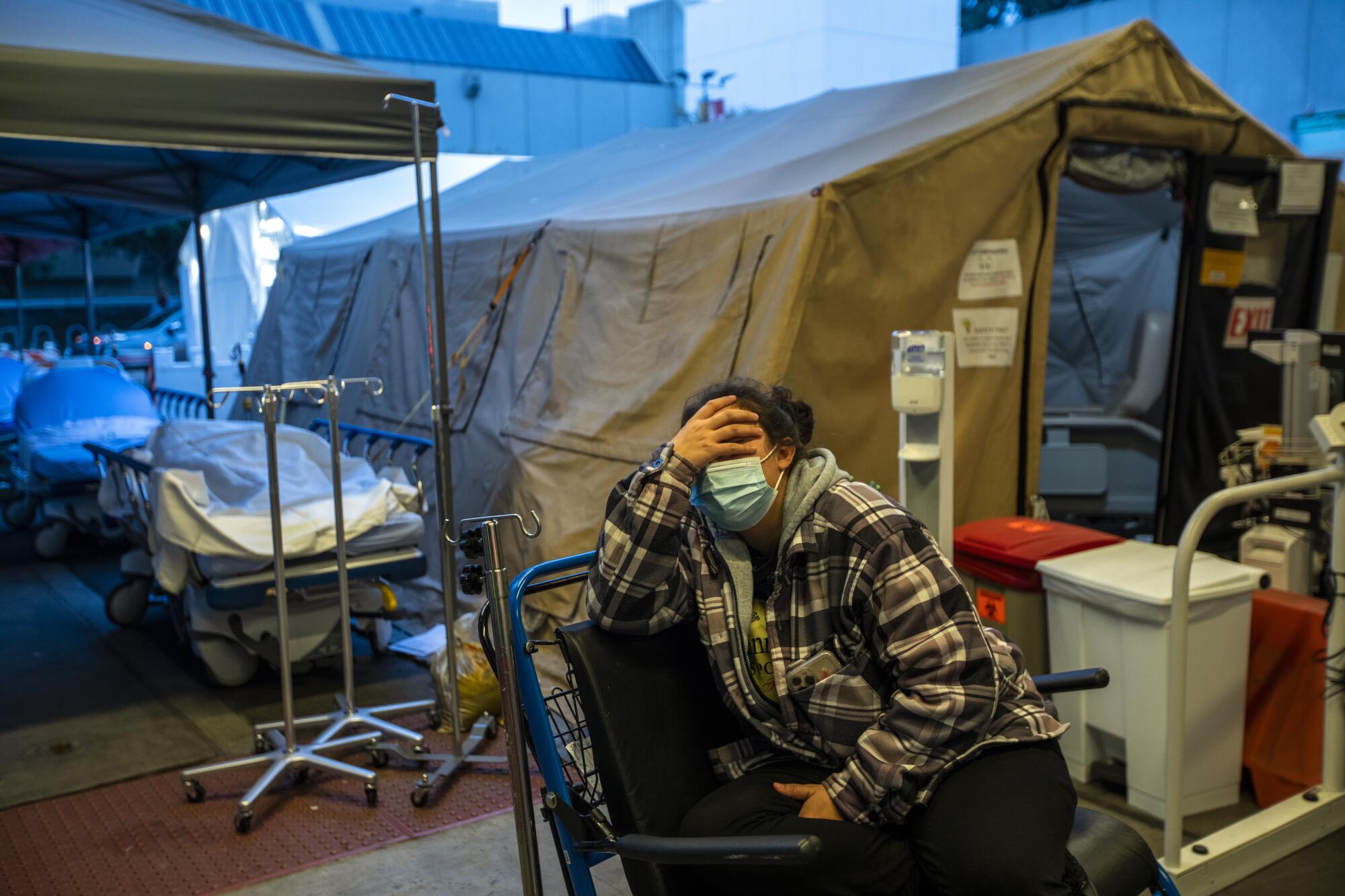
A man with painfully swollen legs from congestive heart failure lies on a gurney outside the emergency room, looking up at a leaden sky that is threatening rain. A wife helps her husband into a triage tent, after his dialysis center refused to admit him after a positive coronavirus test.
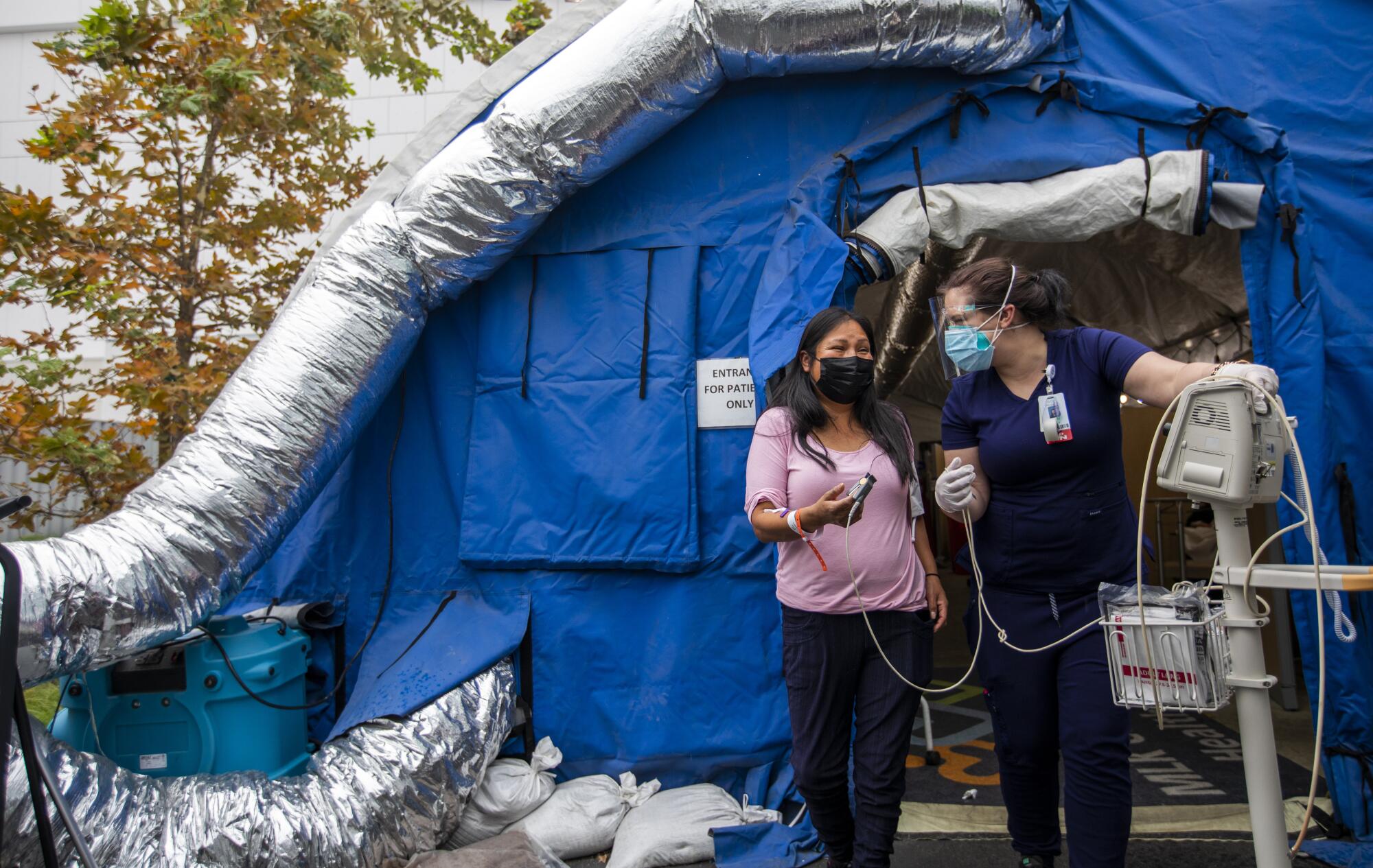
Arriving at the emergency department of Martin Luther King Jr. Community Hospital, people are treated in field tents, hallways, cubicles, former administrative offices and ambulance bays. Many wait in the open air with coughs and sore throats to get tested for the coronavirus. Others come for all sorts of chronic diseases that perpetually curse South Los Angeles.
A year ago, MLK was arguably ground zero for hospitals besieged by a brutal COVID-19 winter surge.
Today, it finds itself in a place both strange and familiar during this surge of the incredibly infectious Omicron variant: overcrowded, often frantic, but under control for an institution accustomed to dealing with the gusher-like confluence of social and medical woes.
COVID-19 was particularly lethal here last year because of the underlying poor health of the community. But the numbers of patients were offset because non-COVID-19 patients stayed away out of fear of catching the virus. The main crunch was in the intensive care unit.
This time, hospital officials say, the virus is more widespread but not as deadly. That has flooded the emergency room with people who are not as sick, and whose preexisting conditions have been exacerbated by the virus.

Dr. Elaine Batchlor, the hospital’s chief executive, said this month that only Antelope Valley Hospital had a higher ratio of patients per bed in Los Angeles County.
But she noted that the everyday, pre-pandemic reality here was only different by a matter of degree: The emergency department generally sees almost three times the number of patients it was designed for.
Before COVID-19, administrators had to convert the ER waiting room into cubicles to treat more patients, and move the waiting room into heated and air-conditioned tents in the ambulance bay. Three more field hospital tents were donated during the pandemic — but they will likely be needed even as COVID-19 cases wane.
“We’ve been a battlefield hospital from the beginning,” said Gwen Driscoll, spokesperson for MLK. “So we know how to handle volume.”
During this surge, most COVID-19 cases are mild enough that patients are tested, given medication and released. But given the sheer number of people coming in, the hospital is full. And like other facilities, it is short-staffed, as the coronavirus is infecting healthcare workers throughout the state.
Even as the winter Omicron surge flattens, Los Angeles County health officials are urging the public to continue avoiding nonessential gatherings.
The result is a kind of fast-moving turnstile for most COVID-19 patients, with long stays mostly for the unvaccinated, who are more acutely ill.
“We’re seeing a lower percentage of people being admitted to the hospital,” said Batchlor. “We’re seeing shorter lengths of stay.”

The lack of adequate health insurance in South L.A., and a dearth of doctors, forces residents to rely on the emergency room for ailments that are otherwise largely untreated, such as heart, kidney and lung disease, stroke, diabetes, and mental illness.
The emergency department was designed to treat 40,000 patients a year when it opened in 2015. Before the pandemic, it was seeing up to 110,000.
“We wouldn’t be like this today if our community had appropriate access to medical care,” said Batchlor. “The reason all these people are in our emergency department now is because there is nowhere else to go. ... Yes, it’s COVID now, but it’s COVID on top of these fundamental disparities in access.”
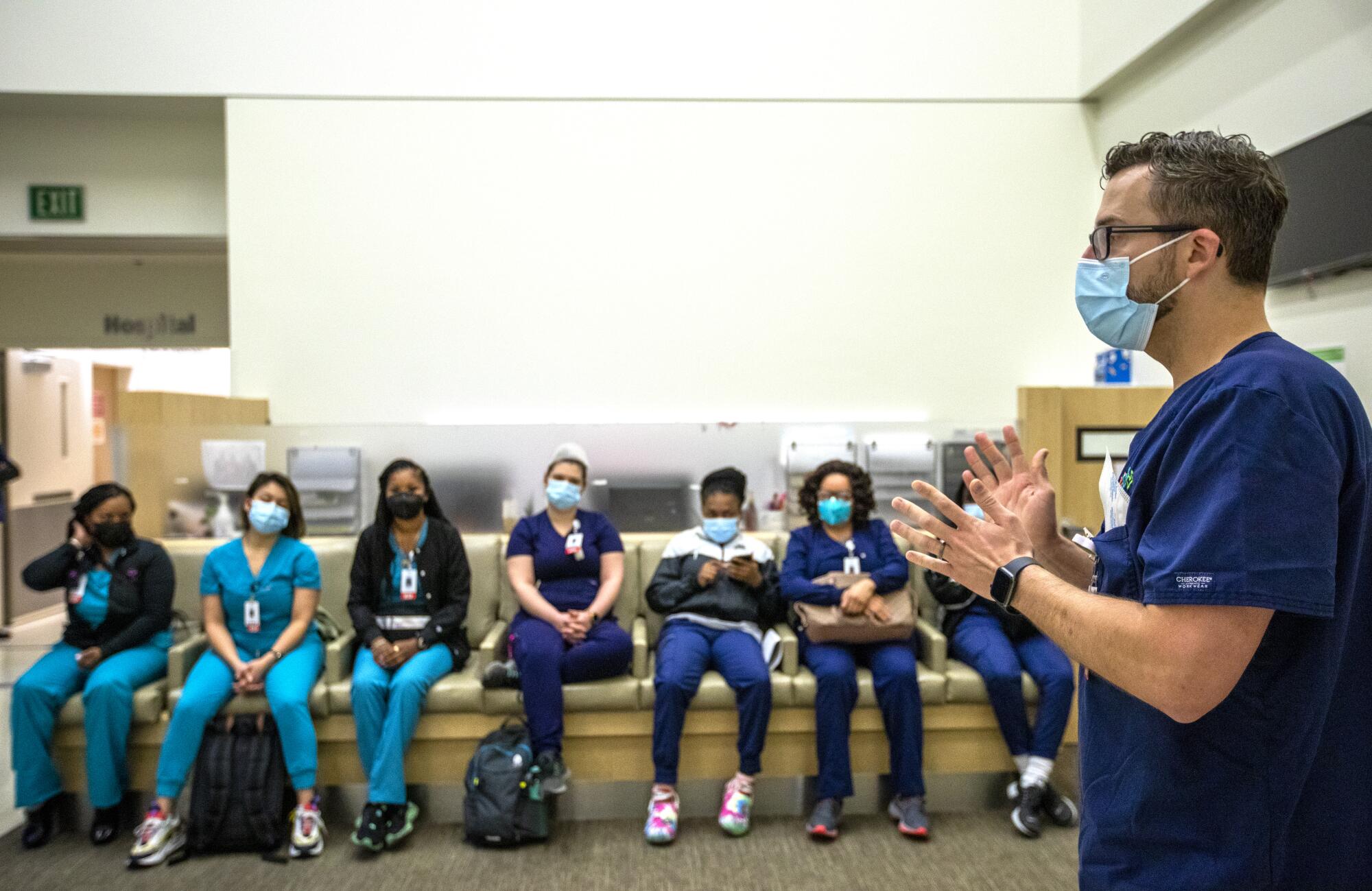
Jordi Gonzalez, nurse manager for the emergency room, started one morning at 6:30 this month with 25 patients from other departments in ER beds, leaving only four open.
“Because we are boarding as many as we have this morning, we are pushing out in the hallways,” he said. “Obviously it’s not ideal to be in the hallway here.”
There are other factors leading to the crowding: COVID-19 patients need to be isolated to keep the virus from spreading, taking up valuable rooms. And during this peak, it has been difficult to transfer people to skilled nursing and mental health facilities, which are also short-staffed but not required by law to take new patients, as emergency departments are.
The early morning is the quietest time of day. “Our volume will explode between 7 and 11 a.m.,” Gonzalez said. They usually don’t clear out the waiting areas until 3 or 4 a.m. the next day.
At 7:30 a.m., people started streaming in, many with COVID-19 symptoms.

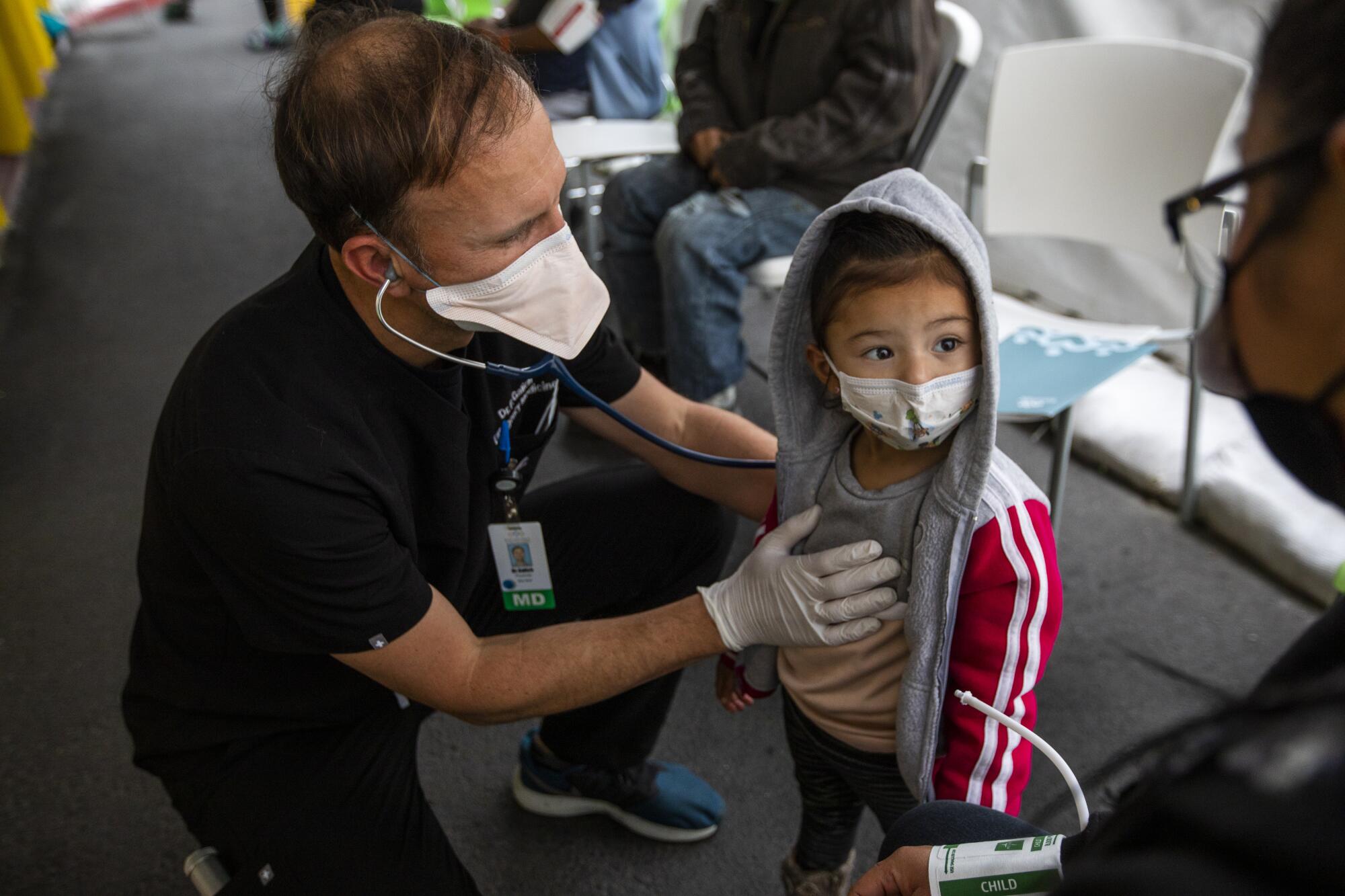
Latima Russell, 37, brought her son Aaron into the triage tent to see a doctor and get tested for the virus. He’d had a bad cough for three days, and her back was aching. They went to St. Francis Medical Center the day before and waited more than seven hours without ever seeing a nurse.
“They didn’t do a test or nothing. I just left,” she said. “Here they get you in and get you out.”
A nurse did an initial triage assessment to determine how serious their cases were within five minutes. They were transferred to some chairs outside the ER, where a nurse came out with a swab to test Aaron.
“OK, buddy, I only need to be in your nose for about 10 seconds in one nostril,” she said.
He turned his head, teared up and started crying before she could count to two. A doctor checked him. His oxygen level was normal, and other vital signs were good. He wrote the mom a prescription for an over-the-counter Tylenol elixir, so that her Medi-Cal plan would pay for it, and off they went.

Jahnee Desselle, 32, sat in the same area outside waiting to see a doctor, while more acute patients were transferred inside. She had body aches, chills and labored breathing that kept her up all night. She is unvaccinated, insisting her religion does not allow the inoculations. She had just got back from a family reunion hunting alligators in Louisiana and, if she were to test positive, suspected she got the virus there.
Dr. Adam Ash approached.
“What’s going on?
“I woke up this morning having a hard time breathing. For the last couple days, my chest has been hurting. And I had a real bad ear ache and a sore throat. I’ve been feeling like throwing up, and some chills. It’s been going on for the last week.”
He booked her into the “respiration tent” for further observation.

On Wednesday, the emergency room got access to an adjacent county building to add up to 18 more treatment spaces.
Batchlor hopes the COVID-19 spikes force state legislators to notice the broken system in poor communities of color in California. She largely blames the perennial overcrowding at MLK on Medi-Cal not paying medical providers nearly enough to offer the preventative medical and behavioral health treatment the community needs.
“If they had those things, they would be healthier, they wouldn’t be as vulnerable to COVID, they wouldn’t be as sick when they contract COVID, and you wouldn’t see the crowding that you’re seeing in this emergency department today.
“It’s part of the multitiered healthcare system we have created in this country,” she added, “and communities like this are at the bottom of that system.”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.













