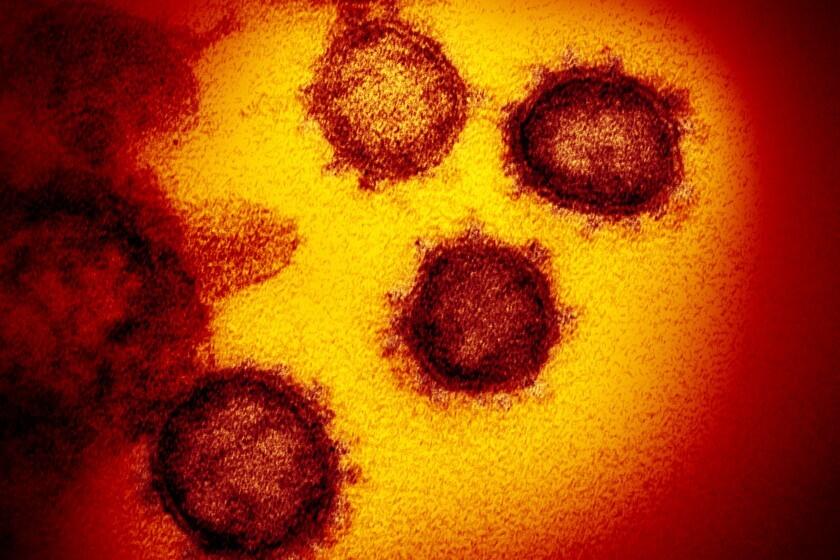
Coronavirus in California is becoming easier to get, much harder to avoid. Here’s why

- Share via
The number of coronavirus cases reported in California is on the brink of crossing 10 million, a milestone that probably undercounts the total significantly yet still carries an increasing sense of inevitability.
Since the hyper-transmissible Omicron variant stormed onto the scene in early December, the virus has wormed its way into seemingly every family and social circle. Residents who for years escaped infection were swept up in the resulting tidal wave of cases, though for many, the severity of illness has been lessened by vaccines, the availability of therapeutics and other factors.
A plethora of high-profile people who have recently tested positive — among them Vice President Kamala Harris, Gov. Gavin Newsom and even Dr. Anthony Fauci — have also fueled the notion that catching the coronavirus is no longer a matter of if, but when.
“It’s going to get easier and easier to get and harder to escape infection. But that doesn’t mean we put ourselves in a sort of mind-set that, ‘You know, to hell with it. I’m just going to do anything I want to do anyway,’” Dr. Peter Chin-Hong, a UC San Francisco infectious-disease expert, said during an interview Friday.
Scientists estimate that nearly 20 million lives were saved worldwide by COVID-19 vaccines during their first year.
It’s understandable that some might view the coronavirus as inescapable, especially amid massive numbers of new infections.
Nearly half of California’s officially reported cases — more than 4.9 million — have been tallied since Dec. 1, the day health officials confirmed Omicron’s presence in California, according to data compiled by The Times.
Officials note those figures are an undercount, and likely a significant one. According to data from the U.S. Centers for Disease Control and Prevention, the most recent seroprevalence estimate for California — the overall share of residents thought to have been infected with the coronavirus at some point — was 55.5% in February.
Still, that means there are likely millions of Californians who have never contracted the virus.
The Omicron strain of the coronavirus keeps generating new subvariants. Here’s a look at how they stack up.
Among those are Chin-Hong, as well as Dr. Robert Wachter, chair of UC San Francisco’s Department of Medicine.
“The fact that I and a fair number of people who continue to be careful and are fully vaccinated and boosted remain COVID-free tells me that it’s possible we will continue to be that way, so I don’t buy the inevitability argument,” Wachter said in an interview Friday. “On the other hand, there are plenty of people who I know who have been just as careful as I have and have gotten it in the past few months, so I think there’s some randomness to this.”
Given the proliferation of ever-more-infectious Omicron subvariants, avoiding the coronavirus has become an increasingly tricky proposition.
“It is likely, as COVID-19 variants continue to evolve to be more transmissible and acquire the ability to evade the protection of antibodies against infection, which results in breakthrough infections in the vaccinated and in those with prior illness, it will be difficult for many to avoid being exposed to COVID-19 going forward,” said Dr. Robert Kim-Farley, an epidemiologist and infectious-disease expert with UCLA’s Fielding School of Public Health.
But infection isn’t inevitable, he added, and “everyone needs to be vigilant to avoid exposure and prevent severe disease,” especially during periods of high community transmission.
“Masking when in crowded indoor settings and being vaccinated and boosted are still the best protections. Also, if one becomes infected and symptomatic, medicines such as Paxlovid will significantly reduce the severity of the disease, especially for persons at higher risk,” he told The Times in an email.
Though there are indications that the latest coronavirus wave may be starting to level off in California, transmission remains elevated. Over the weeklong period ending Thursday, the state reported an average of 16,130 new cases per day — a decrease of almost 12% from two weeks ago, according to data compiled by The Times.
The new infections, however, have not created anywhere near the same level of strain on hospitals as the pandemic’s previous surges. But the number of coronavirus-positive patients is growing steadily.
As of Friday, 3,169 such individuals were hospitalized statewide — up 21% from two weeks ago. The number of patients being treated in intensive care units has likewise crept up, to 331, but that number remains among the lowest of the entire pandemic.
It’s true that not all patients are hospitalized for COVID-19 infections. The California Department of Public Health says about half are there “due to COVID-19 and not simply with COVID-19.” But officials say all coronavirus-positive individuals place demands on healthcare facilities.
“Even though half of these patients may not be hospitalized because they have COVID-19, they still influence hospital workload and burden due to special infection control precautions and placement,” the department told The Times in a statement last week.
Despite the latest surge in coronavirus cases, the impact on hospitals has been relatively minor and COVID-19 deaths have remained fairly low and stable.
But while this apparent script — less severe illness, even during a prolonged period of elevated transmission — is a promising development, officials and experts stress that it’s impossible to predict the future course of COVID-19.
One area of concern is the proliferation of two Omicron subvariants: BA.4 and BA.5. Those are not only highly transmissible, but have shown the ability to reinfect survivors of earlier Omicron strains.
In recent weeks, BA.4 and BA.5 have gradually made up a larger share of new coronavirus infections nationwide. Over the seven-day period ending June 18, the CDC estimated BA.5 accounted for 23.5% of new cases, and BA.4 made up 11.4%.
How the subvariants’ growing footprint will alter the pandemic’s path in California remains to be seen. However, the World Health Organization noted recently that “the rise in prevalence of BA.4 and BA.5 has coincided with a rise in cases” in several regions, and, in some countries, that increase “has also led to a surge in hospitalizations and ICU admissions.”
Three weeks after becoming the first California county to reinstitute a mask mandate in most indoor public settings amid climbing coronavirus cases and hospitalizations, Alameda County has rescinded the order.
It is possible that increases in hospitalizations are simply the numerical byproduct of growing infections. As the WHO noted, current available evidence doesn’t indicate a change in disease severity associated with either BA.4 or BA.5.
“It’s still very early in our experience with BA.4 and BA.5, and so we are monitoring the literature closely to see if there is any data on that,” Dr. Paul Simon, chief science officer for the Los Angeles County Department of Public Health, said during a briefing Thursday. “And certainly, if we do see anything, even a slight increase in virulence for BA.4 and BA.5, that would raise a lot of concern for us and, I think, increase the stakes in terms of encouraging the various protective measures that the public can take.”
Another wrinkle is the recent decision by federal health officials to authorize children as young as 6 months to receive either the Pfizer-BioNTech or Moderna vaccine. While COVID-19 has not hit the youngest children as hard as other age groups, they’ve still been vulnerable to infection — and could potentially spread the virus to others more at risk of severe health issues.
“The fact that kids now under 5 are getting vaccinated, kids 5 and over can get a booster, there’s more Paxlovid going around, all of that might keep community viral load lower than it would have been,” Chin-Hong said.
Both Pfizer and Moderna are considered safe for kids of all ages, but here are a couple of differences that parents can consider.
But at this point, the coronavirus is still widely circulating. And each infection carries with it not just the chance of near-term health impacts, but the risk of developing “long COVID,” in which symptoms can linger for months.
That’s a possible outcome with which Wachter is all too familiar. His wife is still grappling with fatigue and some brain fog weeks after she was infected.
Some who develop long COVID, he said, will have prolonged symptoms that are “life-limiting in a way.” For others, those “will actually be disabling.” In either case, residents shouldn’t ignore the possibility.
Another symptom recently infected people should be wary of is guilt — a feeling that catching the coronavirus somehow indicates they made a bad decision and are now paying the price.
“It’s not a moral failure,” Chin-Hong said. “There are a lot of reasons why it’s so easy to get this particular infection, even when you’re taking a measured approach to life.”
Following the decision by federal health officials to authorize children as young as 6 months to receive the COVID-19 vaccines, Californians are able to book appointments for their tiniest charges.
After all, people still have to go to work, run errands and take care of their children or other relatives should they become ill. And many are now taking the opportunity to resume activities they either weren’t able to do or didn’t feel comfortable doing earlier in the pandemic.
“We’re humans. We’re social creatures. We were meant to get out and do things,” Wachter said. “All of us have to make choices about the level of risk that we’re willing to take. And that’s true when we get up and get out of bed in the morning; it’s true when we get on an airplane; it’s true when we get in the car.”
That’s not to say that precautions like masking in crowded indoor settings and getting vaccinated and boosted, when eligible, don’t still make sense. But Californians needn’t beat themselves up if they take those steps and still fall prey to the coronavirus.
“There are many people who are getting infected who are remaining super careful,” Wachter said. “That’s the thing now, even very cautious behavior is no guarantee you’re not going to get it. This damn thing is so incredibly infectious.”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.