Wastewater data shows big coronavirus spike in San Diego

- Share via
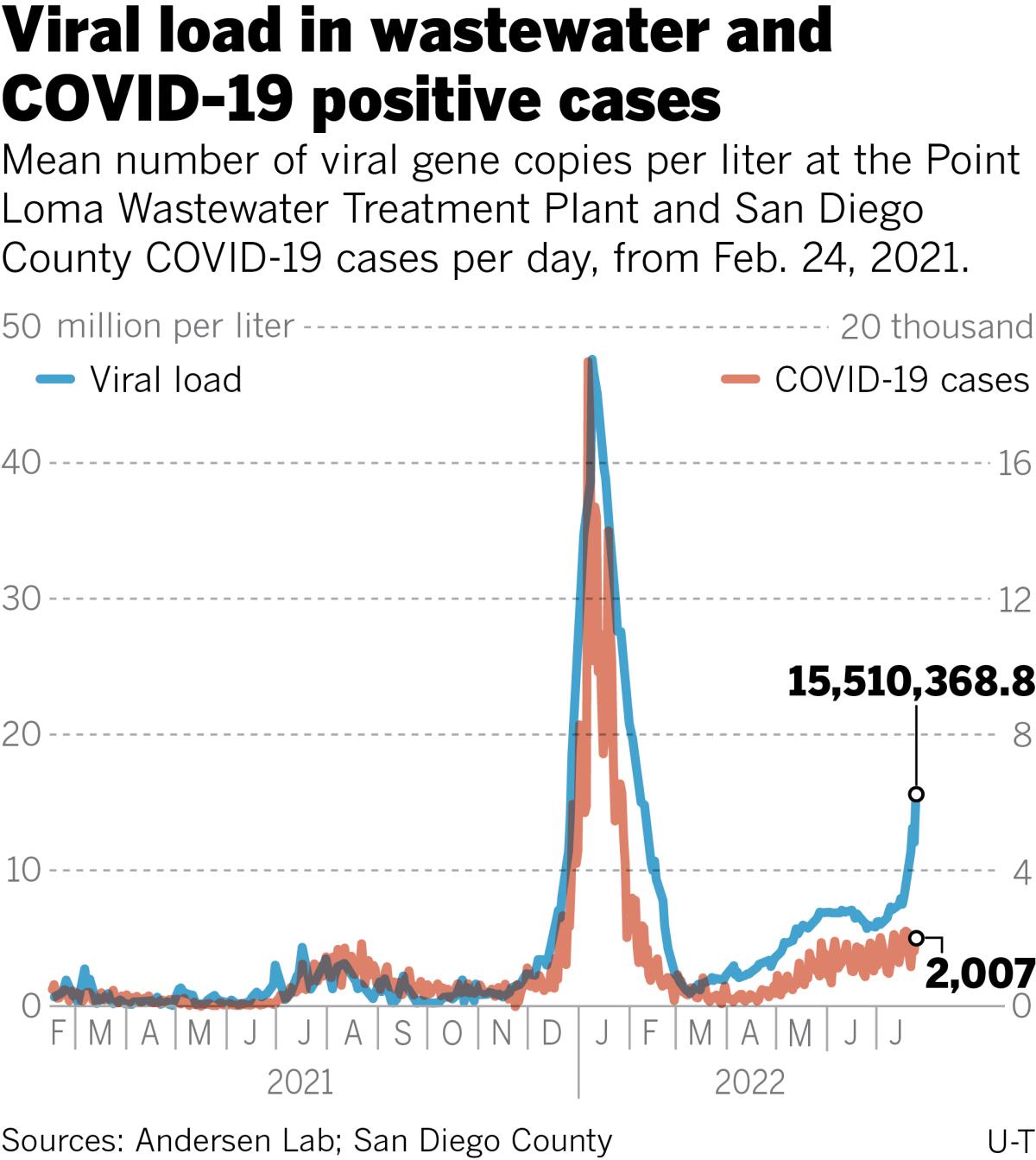
SAN DIEGO — San Diego’s latest wastewater numbers show that the region is experiencing a massive increase in coronavirus transmission driven by BA.5, the subvariant now causing concern worldwide.
Updated Thursday by the SEARCH Coalition, a group of local research labs led by UC San Diego and Scripps Research, wastewater testing detected 15.5 million coronavirus copies per liter of wastewater sampled at the Point Loma treatment plant on Wednesday. It’s a score that is almost double the 8 million copies per liter detected in the same sampling location one week earlier.
The trend visible in wastewater is starkly different from the one depicted by the latest testing data released by the county health department Thursday. Comparing the same Wednesday-to-Wednesday period, positive test results reported to the health department fell 8.3%, from 2,191 to 2,007.
“We have every expectation that cases are eventually going to start rising the same way,” said Dr. Cameron Kaiser, deputy public health director for San Diego County.
At the moment, he added, everyone is advised to do all they can to help slow the spread. Even though there is not currently a statewide mask mandate, wearing a mouth covering, especially in situations where many people are gathering together, is strongly advised.
“We want everyone to step up; we want folks to get their shots and consider the events that they have to do and the events that they don’t,” Kaiser said. “We want the general public to get that good quality, well-fitting mask out and put it on.
“The preponderance of the evidence shows that masks work, and we need to break the cycle of transmission.”
Wastewater is currently thought to be a better indicator of the true amount of virus circulating in a community because many who take at-home tests don’t share their results with local health departments and because the virus is shed into a community’s sewers even by those who are infected but who have no symptoms that would cause them to get tested.
The first Omicron wave that began in December 2021 crested at 47.6 million coronavirus copies per liter of wastewater on Jan. 9.
Whether the current surge will equal or surpass such heights is anyone’s guess, though the situation on the ground is much different today There’s no indoor mask mandate in place (though some counties could soon impose them) and large community events are back on social calendars to a much greater extent than was the case this past winter.
Many are starting to again liken the coronavirus to the flu, suggesting that an overall drop in mortality from COVID-19 due to vaccination and better treatment options have removed the pandemic’s most severe threat. But Kaiser disputed that conclusion, noting that while mortality rates definitely are much lower than they were in 2020 and 2021, they are still greater than would be expected with the flu.
“BA.5 is certainly capable of killing,” Kaiser said. “We’ve had at least 33 San Diegans die of COVID in June which is when BA.5 started to become more dominant.” He pointed out that all 33 deaths were caused by COVID and that count did not include those patients who had tested positive for the coronavirus but died of other causes.
Dr. David “Davey” Smith, chief of infectious diseases at UC San Diego, said the current level of community activity suggests that viral transmission will continue to increase, a reality that should cause individuals to reassess their risk of infection and reinfection. It is clear that infection over the winter in the first Omicron wave is no guarantee of protection against BA.5.
“Even if you’ve been vaccinated, infected, boosted — all of those — [it] doesn’t mean you are immune to the current variant,” Smith said.
The true consequence of coronavirus reinfection is currently being studied, but Smith said there are indications that it could increase the chances of severe health consequences.
“You should try to dodge COVID as many times as you can, because it looks like getting repeated infections is probably not good for your health,” Smith said.
Does that mean canceling planned events as July bleeds into August? The translational research virologist said that he prefers a “harm reduction” strategy that emphasizes outdoor events, masking indoors and in heavy crowds and plenty of social distance where possible.
“I’m not a cancel person, I’m a ‘Let’s take some precautions’ person,” Smith said.
Precautions, he added, should be at their most pointed when interacting with people who are vulnerable. Those with underlying health problems such as diabetes, those with compromised immune systems, and those who are older all are at increased risk of ending up in a hospital bed if they do get sick.
“If you’re getting ready to go visit Grandma who has a lot of issues, and you’re coming from a big event, it may not be the best time to have that exposure,” Smith said. “Test before you go visit Grandma.
“You might be feeling well, but you could be asymptomatic. That’s the danger because, if you have it, you’re going to give it to Grandma when you go visit, even if you don’t feel it.”
Confirmed and suspected COVID-related hospital admissions have continued to climb at nonmilitary hospitals in San Diego County, reaching 479 Wednesday, 69 more than one week ago.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.










