COVID-19 and flu cases are rising in California. How bad will the holiday uptick be?

COVID-19 and flu are rising across California, sparking new warnings from health officials to take precautions as the wider winter holiday season looms.
The uptick is modest and not wholly unexpected — wintertime surges have been an annual occurrence since the coronavirus first emerged. But experts say lagging uptake of the latest reformulated vaccines has left some populations particularly vulnerable to severe health outcomes that are largely preventable at this point.
Over the week that ended Dec. 9, 2,449 Californians were newly admitted to hospitals with a coronavirus infection, up 40% over the last month, according to federal data.
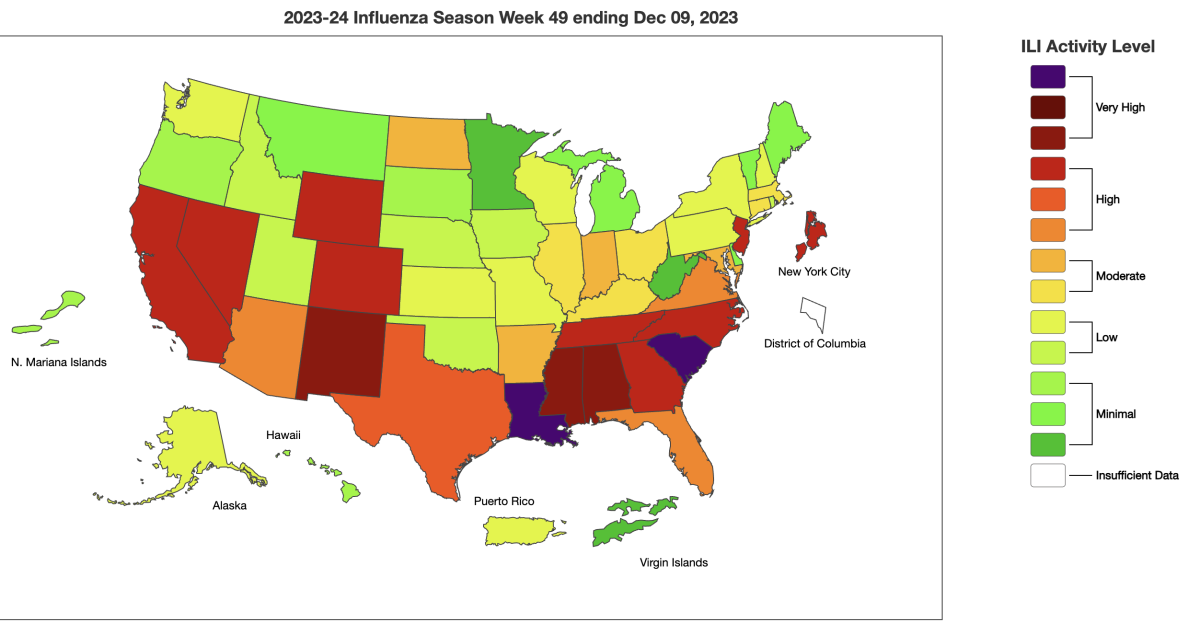
California was considered to have “high” viral illness activity level as of Dec. 9, among the worst designations in the country, the U.S. Centers for Disease Control and Prevention said.
“Respiratory illness activity is rapidly increasing across the United States,” the CDC said in a bulletin Thursday afternoon. “Millions of people may get sick in the next month or two, and low vaccination rates mean more people will get more severe disease. Getting vaccinated now can help prevent hospitalizations and save lives.”
A rise in viral illness is expected this time of year, but the prevalence of COVID-19 adds a considerable health burden that didn’t exist before the pandemic. COVID-19 remains the primary cause of new respiratory hospitalizations and deaths nationally, causing 1,000 fatalities a week.
“COVID is still causing the most number of cases, the most number of hospitalizations and the most, unfortunately, number of deaths that we’re seeing week over week,” Dr. Mandy Cohen, director of the CDC, said in an online discussion Tuesday. “So while we all wish we could leave COVID in the rearview mirror, it is still here with us, and so we need to make sure we are continuing to take it very seriously.”
Cohen last week urged people to take precautions such as getting vaccinated, avoiding people who are sick and staying home when ill, regular hand-washing, improving air ventilation and wearing a mask.
The Centers for Disease Control and Prevention says October is the right time to get vaccinated, before COVID circulation really ramps up.
“And get tested, so you know what you have and you can get treatment,” she said. “Getting tested and treated early can prevent you from getting severely ill, being hospitalized and can potentially save your life.”
Relatively speaking, COVID-19, flu and another ailment — respiratory syncytial virus, or RSV — aren’t at the heights they were this time last year, when their simultaneous circulation spawned a “tripledemic” that stressed healthcare facilities across the state, especially children’s hospitals.
Kaiser Permanente Southern California began noticing more COVID-19 illness starting in mid-November, with the rise accelerating after Thanksgiving, said Dr. Nancy Gin, regional medical director of quality and clinical analysis for the health system.
California’s respiratory virus season is ramping up, prompting officials to renew their calls for residents to get vaccinated in hopes of reducing pressure on hospitals.
Coronavirus levels in Los Angeles County wastewater were at 38% of last winter’s peak for the week that ended Dec. 2, the most recent data available. That’s exactly the same as the height seen late this summer, when the region experienced a prolonged uptick in infections.
The latest figure signals a “medium” level of concern, as defined by L.A. County health officials.
In the San Francisco Bay Area, coronavirus levels in the San Jose watershed’s sewage have been at a “high” level for weeks.
Rising viral levels in wastewater is “like the canary in the coal mine,” said Dr. Peter Chin-Hong, a UC San Francisco infectious diseases expert. Higher concentrations could be followed by more illness, potentially severe enough to require hospital care.
“I’m just worried that it’s going to translate into hospitalizations around Christmastime,” he said.
Some pregnant patients who were eager to get vaccinated to protect their babies against RSV instead met with obstacles.
Chin-Hong said he’s particularly concerned about seniors who haven’t received their updated vaccinations this autumn. Among Californians ages 65 and older, just 27% have received the latest COVID-19 vaccination that became available in September. Uptake is even lower in Los Angeles County — 21% — but higher in the Bay Area, where it’s around 40% in the most populous counties.
Seniors who have not gotten the latest vaccine are “the population we’re seeing in the hospital,” Chin-Hong said, and, especially those who are older than 75, “the population that’s dying.” It’s also likely that many of those who are dying aren’t getting anti-COVID drugs in time.
Flu vaccination rates are slightly lower than they were at this time last year, according to data shared by the CDC. As of early November, 36% of U.S. adults had received their flu shot, compared with 38% at that time last year. And for RSV, just 16% of adults ages 60 and older had received the newly available vaccine as of Dec. 2.
Alarmed by low vaccination rates, the CDC issued a health advisory on “the urgent need to increase immunization coverage for influenza, COVID-19 and RSV.” The agency asked healthcare providers to strongly urge immunizations, noting that “low vaccination rates, coupled with ongoing increases in national and international respiratory disease activity ... could lead to more severe disease and increased healthcare capacity strain in the coming weeks.”
The new COVID shot is available at CVS and Walgreens at no cost through most insurers. But Kaiser enrollees must wait until Sept. 28 to avoid paying out of pocket.
The CDC recommends virtually everyone ages 6 months and older get the latest flu and COVID-19 vaccinations. Adults ages 60 and older are also eligible to be vaccinated against RSV, which can be especially risky for older people with heart disease. There are two vaccines available for older adults: Abrysvo, made by Pfizer; and Arexvy, made by GSK.
The CDC also recommends the Abrysvo vaccine for pregnant people and immunizing babies against RSV with an antibody known as nirsevimab, also known by the trademarked name Beyfortus.
The agency is also urging doctors to recommend antiviral drugs for flu and COVID-19, such as Tamiflu and Paxlovid, for eligible patients. These “antiviral medications are currently underutilized, but are important to treat patients, especially persons at high-risk of progression to severe disease with influenza or COVID-19, including older adults and people with certain underlying medical conditions,” the CDC said.
Such antiviral drugs “are most effective in reducing the risk of complications when treatment is started as early as possible after symptom onset,” the CDC said.
Amid controversies over stay-at-home and masking orders, a lasting difference between Govs. Gavin Newsom and Ron DeSantis’ approach may end up being rhetoric on vaccine safety.
So far, hospitals in Southern California and the Bay Area appear to be in fairly stable shape. More people are becoming ill, but so far, many aren’t needing to be hospitalized, Chin-Hong said.
Kaiser Southern California has been noticing more people ill with COVID-19 in its clinics and urgent care centers, “but they’re not landing in the hospital nearly as much compared to last year, certainly compared to two years ago,” Gin said. “Time will tell if the numbers that we see continue to go up.”
The health system, which serves 4.8 million members and operates 16 hospitals throughout the region, has observed a bit of a rise in the use of ventilators and intensive care units related to COVID-19, “but it’s certainly nothing dramatic,” Gin said.
But cases of influenza type A virus nationally “are really shooting up quite a bit. We are seeing that as well,” Gin said.
U.S. health officials say at least seven states are seeing high levels of the flu and that cases are rising in other parts of the country.
As for RSV, levels rose steadily from the end of September through mid-November. In the last few weeks, however, that virus seems to have flattened out at “less than half of what we saw last year at this time, at least by our testing numbers. So that’s a good sign,” Gin said.
Increasing coronavirus transmission is probably being assisted by waning immunity from past infections and older booster shots.
Officials are also monitoring the rapid rise of the JN.1 subvariant. Because of its unusually high number of mutations, this subvariant — described as a closely related offshoot of the BA.2.86, or Pirola strain — might be able to more easily infect people who had previously caught an older version of the coronavirus or haven’t yet received an updated shot.
Nationally, JN.1 is estimated to account for about 21% of coronavirus cases for the two-week period that ended Dec. 9, up from 8% in the prior two-week period. It’s the fastest-growing subvariant being tracked.
Ron DeSantis cited a scientific journal as evidence Florida had a lower COVID death rate than California. The study’s author says that’s not the whole story.
JN.1 is on the ascent while the current most dominant subvariant, HV.1, is declining. A descendant of the XBB subvariants that were dominant over the summer, HV.1 was estimated to account for 30% of coronavirus specimens for the most recent two-week period, down from 32% in the prior comparable period.
The rise of the new subvariant should encourage people, especially those who are older, to get the new vaccine, as outdated booster shots or natural immunity from past infections may not be protective enough. The new vaccine will replenish antibodies, Chin-Hong said, which will be especially important for at-risk people.
“Most people have gotten a previous infection, like during the summer, with one of the XBBs,” Chin-Hong said. The rise of JN.1 “just makes the clock tick faster before they’re more susceptible [to another coronavirus infection]. In other words, if the XBBs were the main game in town, you might have had a little bit more time before you would get infected again.”
The CDC said available vaccines, tests and antiviral medication continue to work well against JN.1.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.


















