Cancer and the bacterial connection

IN the 1890s, a New York surgeon named William Coley tested a radical cancer treatment. He took a hypodermic needle teeming with bacteria and plunged it into the flesh of patients.
After suffering through weeks of chills and fevers, many showed significant regression of their tumors, but even Coley himself could not explain the phenomenon.
His experiments were sparked by the observation that certain cancer patients improved after contracting infections. One patient experienced regression in a tumor in her arm after developing Saint Anthony’s fire, a streptococcus skin infection.
Doctors at the time considered Coley’s bacterial mixtures to be more black magic than medicine, and with the advent of radiation therapy, the well-meaning doctor was soon consigned to the annals of quackery.
But today, some scientists think Coley had it right: Germs can teach our bodies how to fight back against tumors. Dr. John Timmerman, a cancer immunotherapy expert at UCLA’s Jonsson Cancer Center, says this revolution has produced “the most exciting sets of compounds in cancer immunology.”
These scientists have not yet proved their case. But new studies are revealing that certain cancers may be reduced by exposure to disease-causing bacteria and viruses, and pharmaceutical companies are testing anticancer treatments that capitalize on the concept by using bacterial elements to boost the body’s natural immunity.
The studies also imply that our cleaner, infection-free lifestyles may be contributing to the rise in certain cancers over the last 50 years, scientists say, because they make the immune system weaker or less mature. Germs cause disease but may also fortify the body, a notion summed up in a 2006 report by a team of Canadian researchers as “whatever does not kill me makes me stronger.”
Almost a century after Coley, in the 1980s, dermatologists began noticing that patients with severe acne, which is caused by another type of bacterium, have reduced rates of skin cancer, lymphoma and leukemia. According to a paper by Dr. Mohammad Namazi at the Shiraz University of Medical Sciences in Iran, studies showed that these bacteria, when injected into animals, appear to stimulate the immune system and shrink tumors.
More recent evidence for this phenomenon comes from studies on cotton and livestock workers, who are constantly breathing endotoxins, a component of bacterial cell walls that causes swelling of lung tissue.
In reports published in the last two years, Harvey Checkoway, a University of Washington epidemiologist, has found that female cotton workers in Shanghai have a 40% to 60% lower risk of lung, breast, and pancreas cancer than other factory workers.
Other recent studies by Giuseppe Mastrangelo at the University of Padua in Italy found that dairy farmers exposed to high levels of manure dust are up to five times less likely to develop lung cancer than their colleagues who work in open fields.
For the dairy farmers and cotton workers, “it’s good news and bad news,” Checkoway says. They have lower rates of cancer but tend to have higher rates of other respiratory problems. Sniffing cotton dust or inducing pimples is never going to be a therapy, he says, but studying the body’s reactions to bacteria could explain why cancer rates go down upon endotoxin exposure. And that might help in developing anticancer drugs.
Dr. Arthur Krieg, chief scientific officer of the Boston-based Coley Pharmaceutical Group, thinks the success of Coley’s toxins comes largely from a difference between DNA of humans and bacteria and viruses.
In 1995, Krieg was at the University of Iowa working with strands of DNA created in the lab, hoping to find a way to turn off genes involved in the autoimmune disease lupus. To his surprise, this DNA stimulated the immune cells he was studying in lab dishes. “I got interested, and I got puzzled,” he says.
His synthetic DNA contained several regions called CpGs. In humans, that region has a kind of chemical “cap” on it, but bacteria -- and Krieg’s synthetic DNA -- lack that cap. Thus, in effect, exposure to that CpG makes the body “think” it’s being assaulted by pathogens, and triggers the immune system to shift into attack mode -- and, in doing so, more effectively battle cancer cells.
Krieg saw medical potential: Maybe one could design small drugs with CpGs in them and use them as immunity boosters. After patenting the method, he left his university job and founded Coley Pharmaceutical Group, which was acquired by the New York-based drug company Pfizer in January.
Five years after his discovery, Krieg’s first compound has proved safe in early trials but has not yet been proved effective. Last year, the injected compound failed to increase survival time in a trial of 1,600 lung cancer patients also undergoing chemotherapy. But Krieg thinks it will prove effective in other patients: “It’s just a matter of finding the right way to use it,” he says.
Timmerman is a strong believer in CpGs, and has been using them with the antibody drug Rituximab in his lab research on mice. Finding the right drug combination is key, he says: “It’s very naive to think that a single off-the-shelf immune stimulant is going to magically treat cancer.”
Krieg’s CpG-based chemicals have proved useful in another arena. Because CpGs boost the immune system, they also can enhance certain vaccines. In a trial sponsored by the U.S. Defense Advanced Research Projects Agency, one of Krieg’s chemicals, VaxImmune, accelerated the body’s response to anthrax vaccine by a factor of two -- from 40 days to 20. Other collaborations are exploring using CpG-containing DNA to develop hepatitis B vaccines and anti-asthmatic drugs. (The company has many CpG compounds, four in clinical trials.)
But Don MacAdam, chief executive of MBVax Bioscience in Ancaster, Canada, is not sure that the healing properties of Coley’s fluids are due to a short strand of DNA. “The immune system is very complicated,” he says, “Any of these therapies that are doing one little thing are very likely to fail.”
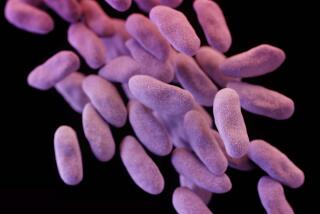
And so MacAdam wants to revive the formulation that Coley himself found most effective -- a mixture of two kinds of bacteria, Streptococcus and Serratia. Such an extract would contain naturally occurring CpGs, endotoxins and other bacterial components that may have therapeutic potential.
MacAdam has solved Coley’s major difficulty: maintaining consistency of the brew from batch to batch. His preparation has been tested on terminal cancer patients outside the U.S. and Canada, and he contends that 24 in 38 patients have shown signs of tumor regression, although nothing is published yet. Dr. Vikas Sukhatme, a professor at Harvard Medical School, says he hopes to run clinical trials once the product has been manufactured according to Food and Drug Administration guidelines.
Other groups have been experimenting with injections of other types of heat-killed bacteria, including Myobacterium vaccae, a tuberculosis relative. In two studies in January’s European Journal of Cancer, researchers report that these bacteria may help fight certain lung and renal cancers.
The first study is a reanalysis of a trial with 162 patients who received heat-killed bacteria (and chemotherapy). In the original study, the treatment didn’t seem to improve survival and in 2004, the company developing the therapy, London-based Silence Therapeutics, gave up on Mycobacterium.
But John Stanford, a shareholder in the company and a researcher at University College London, says these studies were poorly designed and analyzed. When he and collaborators re-analyzed the results, they found that Mycobacterium injections could increase survival of adenocarcinoma patients by four months. Stanford believes that part of the bacterial cell wall switches the body from producing ineffective antibodies to sending out cancer-killing blood cells.
In the second study, researchers reported that 60 renal cancer patients injected with Myobacterium survived just as long as those treated with standard chemotherapy.
Stanford has formed a company, Immodulon Therapeutics, and wants to run trials with a stricter and more intense injection regime, to repeat the results and, hopefully, extend patients’ lives longer.
Although both Krieg and Timmerman are inspired by Coley’s work, they question the philosophy behind reviving Coley’s preparation and using other bacterial extracts. But, Krieg says, “as a physician you have to maintain a sense of humility and avoid being overly skeptical.”