Op-Ed: Lung failure leads to COVID tragedies, but lung disease was a crisis even before the pandemic
- Share via
The World Health Organization reports that more than 5 million people worldwide have died of COVID-19, with numbers rapidly rising again. When we look at how people with COVID-19 die, the most common cause is catastrophic lung failure.
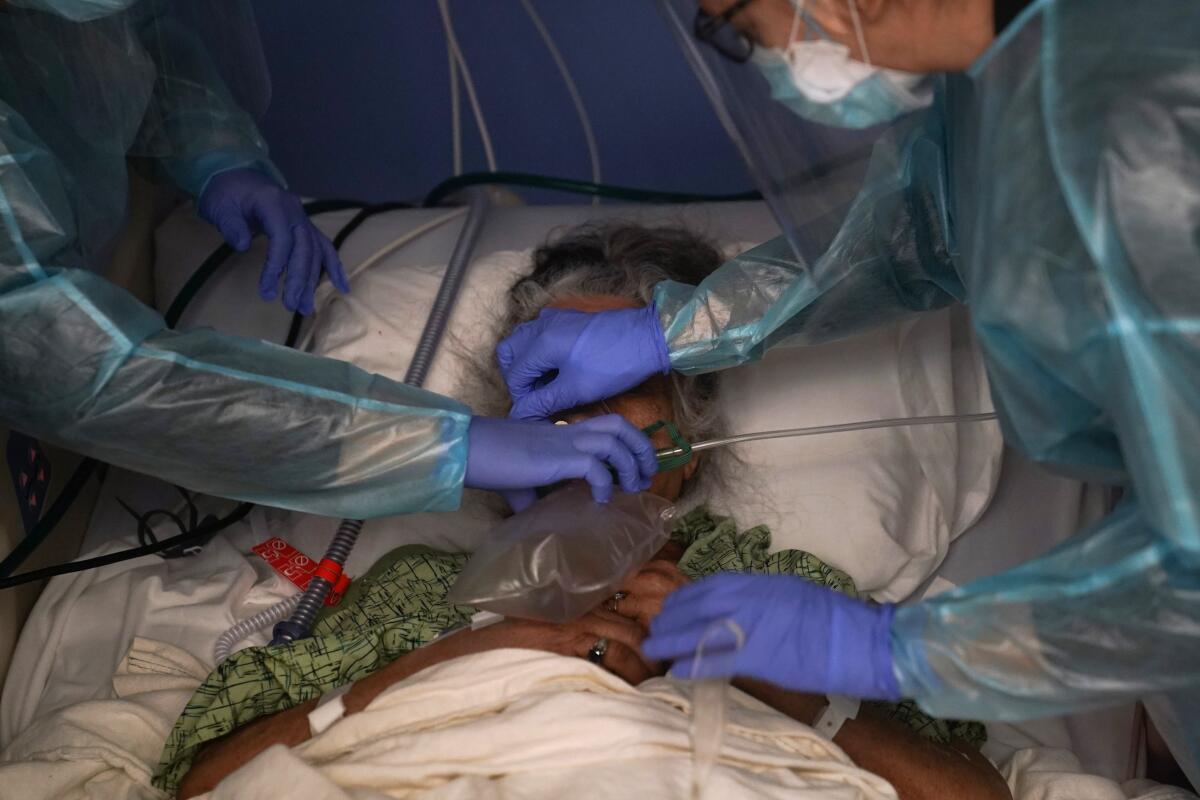
Once the lungs fail, other organs soon follow, like a game of Jenga when the linchpin block is removed. At this stage, even for patients thought to be previously healthy, we cannot stop the virus from wreaking havoc. It’s a painfully familiar script for many admitted to the hospital with minor breathing issues: Blood oxygen levels drop. Supplemental oxygen isn’t enough. They end up on a mechanical ventilator. Days later they are dead.
A respiratory therapist’s view of how the worst cases of COVID fare. They rarely end well.
Despite truly remarkable advances in our capacity to diagnose and treat disease in the 21st century, our ability to treat lung disease is still profoundly primitive — and, intensified by the pandemic, that deficit has tragic results.
The first successful kidney transplant occurred in 1954, followed by liver in 1967 and heart in 1968. The first successful double lung transplant happened in 1986. Yet even now, long-term survival for lung transplant patients lags behind that of other major organ transplants. For instance, the median survival of a lung transplant patient is 5.8 years, compared with 12 to 13 years for a heart transplant patient.
Before the pandemic, chronic lung disease was already the third leading cause of death worldwide, and pneumonia the leading cause of death among children under the age of 5.
Yet we failed to make the kind of strides seen in other diseases. In the latter half of the 20th century, for instance, mortality from cardiovascular disease dropped over 50% in the U.S. following greater research investment, targeted disease prevention and treatments, and clinical trials that led to the development of powerful new medications to manage cholesterol and blood pressure.
We have not adequately invested in lung research. While there are many reasons for research funding disparities, a major factor has been the stigma associated with lung disease, framed as an illness of personal responsibility: If you smoked, you gave yourself lung cancer or emphysema. But health behaviors play a role in many diseases, such as cardiovascular disease and diabetes where diet and exercise contribute.
A federal panel proposes offering lung cancer screening to lighter smokers and those who are slightly younger, greatly increasing the number who qualify.
Even before COVID-19, we had no specific therapies for acute respiratory distress syndrome — the pattern of severe lung injury seen in severe COVID-19. Treatment generally consists of supportive care with mechanical ventilation, which itself can cause lung injury if not properly employed. Nearly 200,000 Americans were dying each year of severe acute lung injury before the pandemic.
Risks to lung health are only increasing. Global air quality is getting worse. Dust and particle pollution are rising due to hotter temperatures and drought. Wildfires are also now driving extremely high particle levels, in some instances miles from the original fire. These exposures induce lung inflammation, contribute to the development of chronic obstructive pulmonary disease and exacerbate asthma.
And these changes ultimately did make COVID more devastating: Research indicated that wildfire exposure in the American West last year resulted in an excess 20,000 coronavirus infections and 750 COVID-19 deaths.
Chronic lung problems may also drive cases of long-haul COVID. My colleagues at the University of Michigan found that some patients now suffering from long COVID had undiagnosed lung inflammation evident on CT scans before they contracted COVID-19. SARS-CoV-2 was fuel for a preexisting fire. Yet unlike blood pressure, we never measure lung function as part of routine care, leading to, for example, an estimated 12 million individuals in the U.S. with undiagnosed chronic obstructive pulmonary disease.
Experts in air quality and pediatric lung health tell how parents can reduce their kids’ exposure to air pollution year-round.
Researchers have also found that a significant proportion of adults diagnosed with chronic lung disease had suffered impaired lung development before adulthood. While we think this damage might stem from factors like premature birth, repeated respiratory infections and secondhand smoke exposure, the truth is we’re not really sure.
But despite an influx of funding for COVID-19 research, shockingly little has gone specifically to understanding lung damage and how to treat it. While vaccines are incredibly important, as are treatments for COVID-19 itself, lung health too must be a national priority. We would never have been able to develop the COVID vaccines so quickly without years of basic science research investment.
Congress and government agencies around the world must appropriate funds for lung health programs including screening, research into mechanisms of lung injury and repair as well as aggressive drug and device development programs.
COVID-19 alone didn’t kill more than 5 million people. It exposed a dangerous failing in medical care. We must recognize the warning signs of lung injury much earlier and prioritize finding ways to prompt recovery.
MeiLan K. Han is chief of pulmonary and critical care at the University of Michigan, a spokesperson for the American Lung Assn. and author of “Breathing Lessons: A Doctor’s Guide to Lung Health.”
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.












