Coronavirus Today: How immune are we?
Good evening. I’m Karen Kaplan, and it’s Tuesday, March 21. Here’s the latest on what’s happening with the coronavirus in California and beyond.
When all mask mandates are gone, and social distancing is long forgotten, and months or even years go by without getting a COVID-19 booster shot, what will protect us from the coronavirus? Our last line of defense is our immune systems.
For most of the pandemic, talking about the immune system has meant talking about antibodies. And with good reason — they’re the proteins that can attach themselves to a familiar viral invader and neutralize the threat until it can be destroyed.
The immune system pumps out armies of antibodies in response to a real coronavirus infection or one simulated by a vaccine. Antibody levels inevitably fall over time, which is why the Centers for Disease Control and Prevention has recommended periodic COVID-19 booster shots. Each jab is like a tune-up for the immune system, prompting it to replenish its antibody supply.
However, getting two or three booster shots a year isn’t a sustainable strategy for fighting COVID-19 over the long term. In addition to the logistics and expense involved, there’s the fact that most Americans aren’t willing to get them. The latest booster shot was rolled out in September, and it’s specifically designed to go after the Omicron variant. Yet as of Tuesday, only 16.4% of Americans have opted to receive it.
Dr. Paul Offit is one of the most pro-vaccine people there is. He’s the director of the Vaccine Education Center at Children’s Hospital of Philadelphia and a professor of vaccinology at the University of Pennsylvania. He serves on the Food and Drug Administration’s vaccine advisory committee. He co-invented a widely used vaccine against rotavirus, an infectious disease that kills an estimated 200,000 children around the world each year. Despite years of harassment from anti-vaxxers, his vocal support for childhood immunizations has never wavered.
Yet Offit has been questioning the wisdom of frequent COVID-19 booster shots for months.
Yes, there’s clear evidence that each dose produces a spike in antibody levels, he says. But it’s temporary. And more to the point, it’s not clear that extra antibodies actually reduce someone’s risk of being hospitalized because of COVID-19 or of dying of the disease, which are the most important things we want the vaccines to do.
What really seems to matter is our T cells. They hunt down cells that have been taken over by the coronavirus and kill them. This “cellular immunity,” as scientists call it, deserves the credit for preventing the worst COVID-19 outcomes, even if it doesn’t stop infections from happening in the first place.
If our plan for keeping COVID-19 in check relies on T cells instead of antibodies, then the vast majority of Americans have no need for repeated booster shots, Offit argues. (An exception could be made for people who are immunocompromised, he says.)
There are lots of reasons to feel optimistic about T cells’ ability to protect us. Unlike with antibodies, their power isn’t undermined by the emergence of new variants. They show up for people with weakened immune systems who aren’t able to mount a strong antibody response.
Perhaps best of all, they don’t seem to fade away as quickly as antibodies do. Remember the 2003 outbreak of severe acute respiratory syndrome, aka SARS? That was caused by a coronavirus called SARS-CoV, which is closely related to the one that causes COVID-19. A 2020 study in the journal Nature reported that SARS survivors still had signs of T-cell immunity 17 years later.
But not everything with T cells is hunky dory. A major problem is the lack of a simple way to measure the state of a person’s cellular immunity — let alone the immunity of the entire population.
Dr. Cody Meissner of Dartmouth College, who specializes in pediatric infectious diseases and sits with Offit on the FDA’s vaccine advisory committee, told my colleague Melissa Healy that scientists are still trying to work out the details of which kinds of T cells do the heavy lifting at any point in time as a patient battles COVID-19. That means “it isn’t easy to look at T cells and ask if we have sufficient numbers of them to protect,” he said.
If you really wanted to gauge a person’s cellular immunity, there are ways to do it. But in most cases, you’d need a lot of money and a large blood sample. The tests are labor-intensive, resource-intensive or both.
If there were a test that could measure cellular immunity as cheaply and easily as other tests measure antibodies, it could be a game-changer. Meissner and others say.
For an individual, this hypothetical test could give a personalized reading on whether a booster shot was necessary. More importantly, if this test could be administered widely, public health officials could use the results to assess whether it was safe to relax COVID rules or if it was time to tighten them. If the coronavirus were to evolve so much that our immune systems no longer recognized it, such a test could detect that too.
One candidate test may be a good start. It doesn’t take a complete census of T cells in a sample of blood, nor does it assess their strength. All it can detect is a genetic signal that a person’s cellular immune system has been activated against the coronavirus. But it can do that in less than a day, and the cost is similar to running a COVID-19 PCR test.
The assay, developed by a British biotech firm, was used last year to assess the cellular immunity of people in Madrid. Researchers determined that a little more than 90% of tested residents still had protection from their cellular immune systems. Among them, the average time since their last dose of the COVID-19 vaccine was about 10 months.
Hyrix, the company that developed the test, would like to offer the test in the U.S. and plans to seek the Food and Drug Administration’s permission to do so. Someday, scientists say, it might be used in concert with other simplified tests to reveal a fuller picture of our coronavirus immunity.
By the numbers
California cases and deaths as of 4:18 pm. on Tuesday:
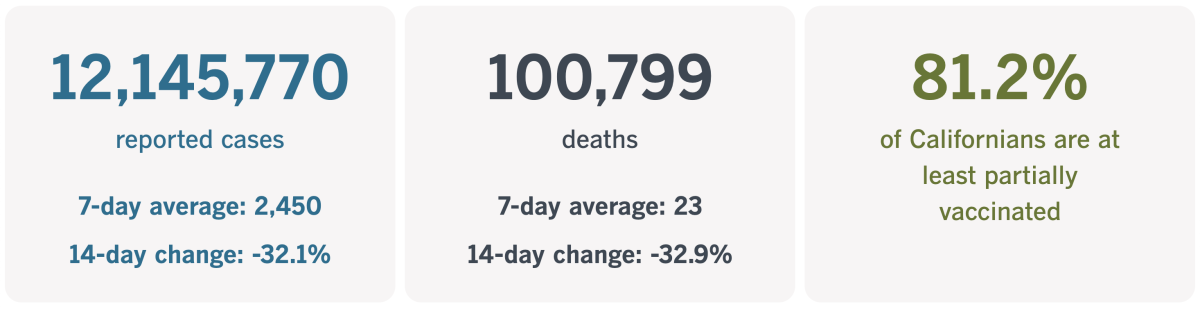
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
What it takes to fight eviction
Meet Leticia Graham. Before the pandemic upended everything, she was getting started in a real estate career focused on upscale renters. She had a fresh license and a spot at an agency in Brentwood. Everything was looking up.
Then the economy shut down. Open houses were canceled. There was nothing for Graham to do except decamp to her own apartment, a modest studio in the Westlake neighborhood that cost her $1,150 a month.
Without work, she fell behind in her rent. Funds from a COVID-19 rent relief program helped a lot, as did a part-time retail job in Glendale. That left her with $2,300 in back rent that she needed to pay off, but despite her thriftiness, she just couldn’t seem to make a dent in it.
In November, Graham found a notice on the door to her studio. It was from her landlord, and it informed her she had to pay her outstanding balance within 72 hours or else find a new place to live.
She knew she couldn’t come up with that kind of money on that kind of timeline. She also knew she wouldn’t be able to find a cheaper housing option. Besides, if she had the kind of money she’d need for a deposit on a new place, she could have used it to pay down her back rent.
No, Graham knew that if she lost her studio, she’d become homeless. She didn’t even have a car she could sleep in until she found a way to get back on her feet.
“I don’t have a place to stay,” the 36-year-old told my colleague Paloma Esquivel.
Graham had been counting on Los Angeles County’s eviction moratorium to keep a roof over her head. She soon learned that belief was misplaced.

After Graham missed the 72-hour deadline, she got a notice to appear in court in February. She wasn’t too worried. Multiple news stories had reported that Los Angeles County’s eviction moratorium had been extended through the end of March, and she took that to mean her landlord couldn’t remove her since the pandemic was the reason she owed rent money.
Based on the conversations taking place between Judge Alison Mackenzie and other renters, Graham wasn’t the only one with an oversimplified view of what the eviction moratorium would do.
Renters were protected only if they owed rent that had been charged since July 1, 2022, and only if they couldn’t pay it because their monthly household income had fallen by at least 10% due to a pandemic-related hardship, among other restrictions, Mackenzie explained.
Indeed, landlords were never prevented from evicting tenants, and although eviction cases dropped from about 3,000 to a few hundred per month, they never stopped altogether. Now they’re back up to pre-pandemic levels, and one researcher at UCLA predicts they could go as high as 5,000 a month.
Tenants who are sued can use the moratorium as part of their defense, but only if they understand how it works and how to present the right kind of evidence. Graham didn’t know either of those things.
When it was her turn to face Mackenzie, the judge strongly encouraged her and her landlord’s attorney to make some kind of deal. Through negotiation, Graham might get a little more time in her studio, or a promise to keep her eviction from becoming public.
Graham and the attorney went back and forth in the hallway but couldn’t come to an agreement. Graham wanted to stay in the studio — and keep paying rent — until July 1, giving herself more time “to get on my feet,” she said. The lawyer wanted her out sooner. The judge asked them to keep trying to find some middle ground.
When they failed again, she sent them back into the hallway to keep talking. However sincere Graham was about saving up more money, it wasn’t a legal defense, Mackenzie said.
“If we go to trial and you lose, you’re out,” Mackenzie told Graham. “I really think you would prefer to find a solution.”
A breakthrough came after Graham asked the lawyer if she could speak directly to the landlord. It took 20 minutes to persuade him to put the eviction proceedings on hold and let her stay through the end of June as long as she kept paying her current rent on time. The deal gave her four months to try to improve her financial situation, perhaps by getting more hours at her retail job or getting back into real estate.
It wouldn’t be easy, but Mackenzie was reassuring as she scheduled a follow-up hearing for July.
“Hopefully you’re going to do everything you need to do so that date I will dismiss the whole case,” the judge said. “It will be like this never happened.”
California’s vaccination progress
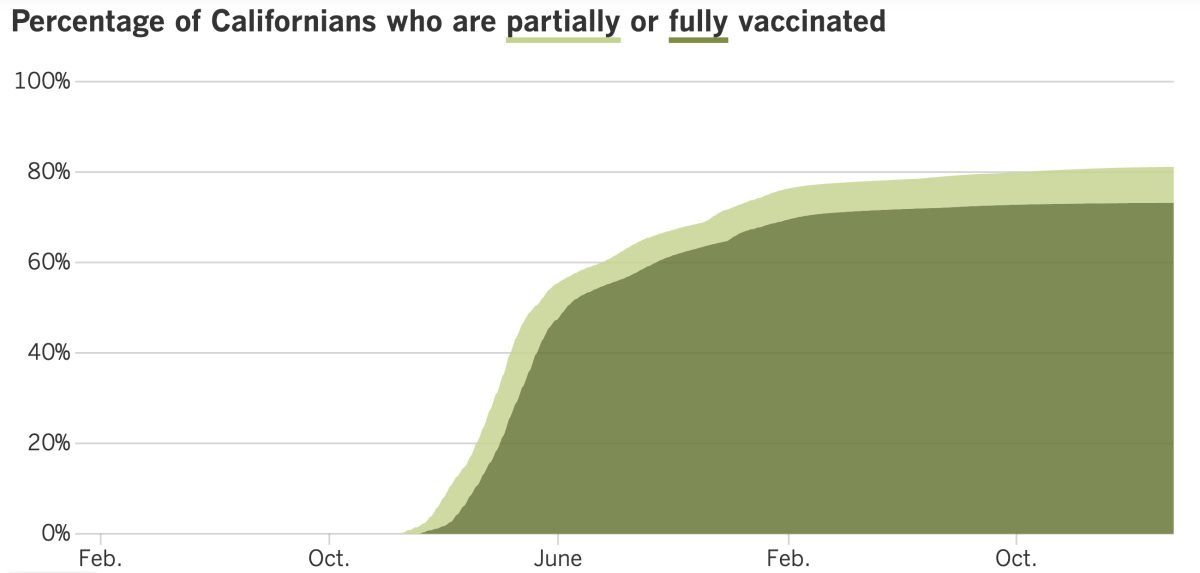
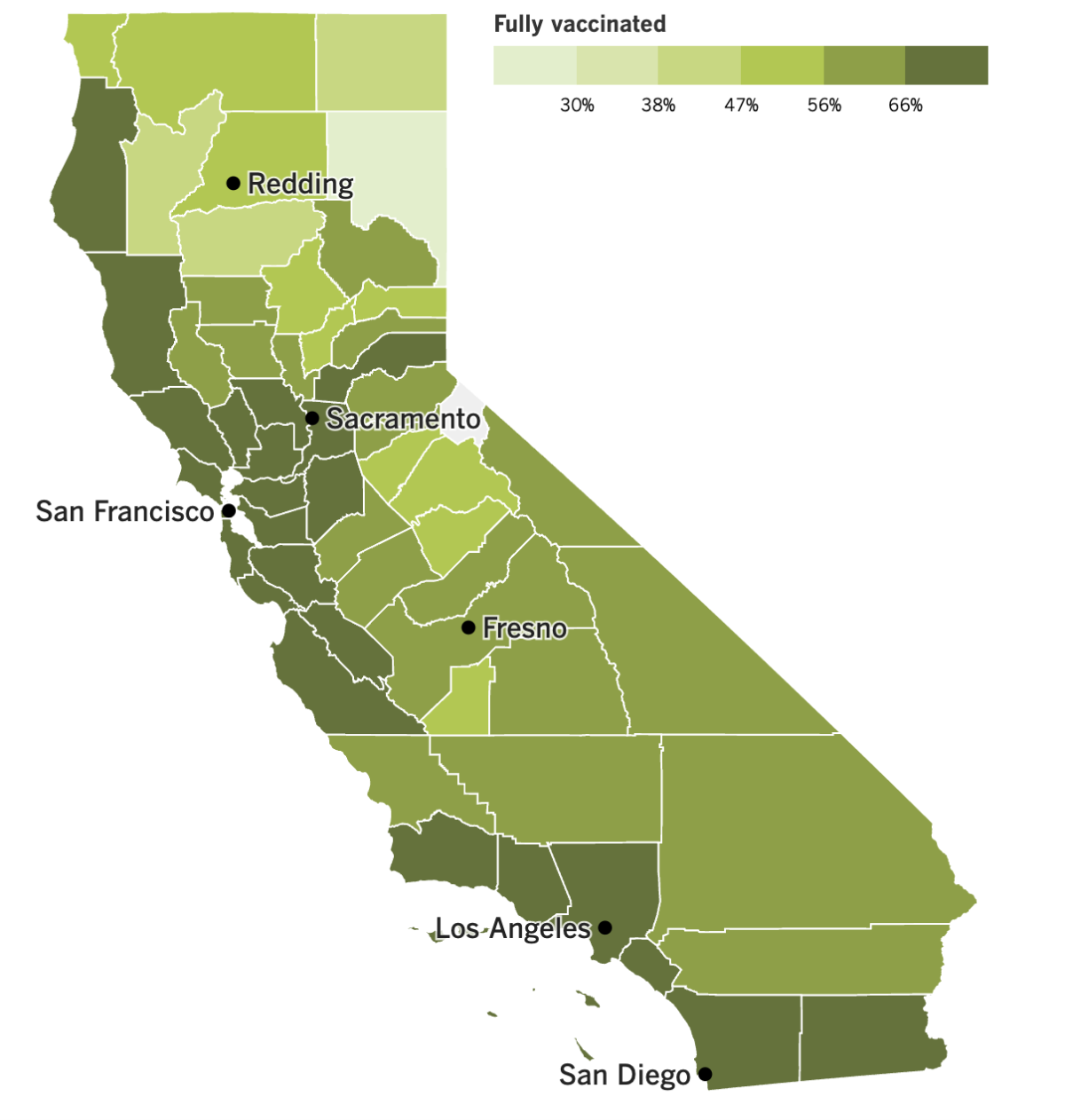
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
I don’t know if rain is bad for the coronavirus, but it kind of seems like California’s massive storms are helping wash COVID-19 away.
The latest map from the CDC reveals that all but four of the state’s 58 counties have low COVID-19 community levels. The exceptions are Sacramento, Yolo, Placer and El Dorado counties, all of which are in the “medium” tier.
Los Angeles County saw a 3.5% decline in new cases week-to-week and a 21% decline in COVID-19 deaths, according to the federal agency. The trends were similar in Orange, San Diego, San Bernardino and Ventura counties. Our own tracker indicates that new cases are down 32% statewide, and deaths are down 33%.
It’s certainly possible that all the storm activity suppressed reporting of new coronavirus infections, but the mortality data is more reliable because deaths are harder to ignore. Statewide, there were 0.4 deaths per 100 residents over the week that ended Sunday, the CDC said.
One tool employed by California’s elected officials to keep the coronavirus in check is a new state law that punishes doctors who spread misinformation about COVID-19 to their patients. The law has been in legal jeopardy since its inception thanks to concerns that its ambiguous language makes it impossible for doctors to know exactly what counts as misinformation, which in turn prevents them from speaking freely with their patients.
As expected, the law prompted a flurry of lawsuits. Now things are even more uncertain because federal judges have issued conflicting rulings in those cases.
One of those judges is in Sacramento, and he temporarily blocked enforcement of the law on the grounds that was “unconstitutionally vague,” among other problems. The other judge, in Santa Ana, declined to issue a preliminary injunction because the law was “likely to promote the health and safety of California COVID-19 patients,” he said. And a judge in San Diego declined to even make a ruling when asked to put the law on hold.
The latter two cases are now in the hands of the federal appeals court, which may agree to block enforcement until the legal issues can be sorted out. However, Gov. Gavin Newsom’s administration has opted not to appeal the Sacramento ruling, preferring to see how the appeals court handles the Southern California cases first.
You may recall that this controversial law has made some strange bedfellows. Among its opponents is a group founded by longtime vaccine skeptic Robert F. Kennedy Jr., and the two doctors behind the Santa Ana lawsuit “have sometimes diverged from public health guidelines,” as our friends at KHN put it. However, many mainstream doctors also oppose the law because they fear it could hinder clear communication with their patients. The American Civil Liberties Union objects to it as well, on free speech grounds.
Speaking of laws, President Biden signed one Monday that will require U.S. intelligence agencies to share a lot more of what they’ve learned about the origins of the pandemic. Specifically, the law directs the Office of the Director of National Intelligence to declassify information about research conducted at the Wuhan Institute of Virology that could have sparked the global outbreak. (There’s an exception for details that could reveal sensitive sources and methods.)
“My Administration will declassify and share as much of that information as possible,” Biden said in a statement.
Another clue about how this all got started appeared last week in the form of genetic sequences that were briefly shared by scientists from the Chinese Center for Disease Control and Prevention. They appear to show that DNA from raccoon dogs had commingled with the SARS-CoV-2 coronavirus at Wuhan’s Huanan seafood market in early 2020. That’s significant because a high percentage of the earliest COVID-19 victims had ties to the market, where live animals were sold.
“These data do not provide a definitive answer to how the pandemic began, but every piece of data is important to moving us closer to that answer,” World Health Organization Director-General Tedros Adhanom Ghebreyesus said last week.
Tedros, who has been calling on China to cooperate more fully with international investigators, said the genetic sequences “could have and should have been shared three years ago.” It’s not clear why they were recently uploaded to — and then removed from — a public database. Luckily, a French biologist noticed them before it was too late and shared them with other scientists who are investigating the coronavirus’ origins.
Their finding — that coronavirus-positive specimens were collected from a market stall that also contained raccoon dog DNA — has not been independently verified or subjected to peer review. If it’s confirmed, it would bolster the idea that the pandemic virus jumped from animals to humans at the market.
“There’s a good chance that the animals that deposited that DNA also deposited the virus,” said University of Utah virologist Stephen Goldstein, who helped analyze the data. “If you were to go and do environmental sampling in the aftermath of a zoonotic spillover event … this is basically exactly what you would expect to find.”
While we’re on the topic of China, it looks as though the country’s official pronouncements that the Communist Party abandoned its so-called zero COVID policy on the basis of “scientific analysis and shrewd calculation” were not entirely truthful. Instead, the government acted impulsively and probably caused hundreds of thousands of unnecessary deaths, the Associated Press reports.
The AP’s conclusion is based on interviews with current and former members of the Chinese CDC, government advisors and other experts, as well as internal reports and directives.
“It wasn’t a sound public health decision at all,” one of the Chinese CDC officials said. “It’s absolutely bad timing … this was not a prepared opening.”
One red flag is that restrictions were loosened just as winter was getting underway, a time when the coronavirus was most likely to spread. In addition, the country’s health system wasn’t prepared for a sudden surge of infections — pharmacies didn’t have antiviral medicines on hand and hospitals didn’t have the supplies or staff they needed — and vaccination rates among older people were still relatively low.
It’s not clear how many people died in the months following the demise of zero COVID. China’s official count is below 90,000, but independent experts estimate hundreds of thousands or even millions of people perished. Models suggest that at least 200,000 to 300,000 of those deaths could have been avoided if the government had made an effort to boost vaccinations and stock pharmacy shelves before lifting its pandemic precautions.
“If they had a real plan to exit earlier, so many things could have been avoided,” said Zhang Zuo-Feng, an epidemiologist at UCLA. “Many deaths could have been prevented.”
And finally, with L.A. County’s COVID-19 emergency coming to an end next week, this newsletter will too. Next Tuesday’s email will be the last edition of Coronavirus Today. But you can rest assured that The Times will continue to cover the pandemic, and you can keep up to date with the developments on our website or via some of our sister newsletters, including Today’s Headlines (which comes out every weekday), Essential California (which publishes Monday through Saturday) and the Health & Science newsletter (which comes out on Saturdays).
Your questions answered
Today’s question comes from readers who want to know: Can I get a prescription for Paxlovid to take with me when I travel abroad in case I get COVID-19 while I’m there?
It is possible for a doctor to prescribe the drug in advance, but your physician may not feel comfortable doing so.
“The decision to prescribe a preemptive Paxlovid prescription is complex,” said Dr. Elizabeth Ko, an internal medicine physician at UCLA.
If you suspect you’ve come down with COVID-19, you’d first have to confirm you have the disease. Other infections can produce similar symptoms, so it would be essential to bring rapid tests with you, Ko said.
Even if your rapid test is positive, you might decide you’re better off without Paxlovid. The pills can cause liver toxicity, and they may interfere with other drugs you take. Your COVID-19 symptoms might not be severe enough to justify those risks — and your doctor may not want you to make that call on your own.
Dr. Edward Jones-Lopez, an infectious disease specialist with Keck Medicine of USC, said that although there are some cases where it’s sensible to bring just-in-case medicines with you when you travel, this is not one of them.
“If we were to supplement every single traveler with Paxlovid, you can imagine how chaotic that would become,” he said.
Jones-Lopez said he would rather advise his patients to get up to date with their COVID-19 vaccinations and take sensible precautions when they’re abroad, such as wearing masks in higher-risk situations.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

The rat in the photo above is crouching on a subway platform in New York City. The picture doesn’t reveal whether he (or she) is infected with the SARS-CoV-2 coronavirus, but a new study confirms that it’s possible.
Researchers gathered up 79 brown rats (Rattus norvegicus) from NYC’s sewer system and tested them for signs that they’d had an encounter with the coronavirus. Thirteen of them had an immune response indicative of coronavirus exposure, and four had active infections. And when the researchers deliberately infected rats under laboratory conditions, the Alpha, Delta and Omicron variants all took hold easily, Melissa Healy reports.
The finding makes rats the 11th non-human species known to carry the coronavirus. (The others are dogs, cats, hamsters, ferrets, deer, mink, otters, gorillas, lions and tigers.) It may sound like bad news for brown rats, but it’s not — infections don’t seem to make them very sick, and none of the rodents in the study died of COVID-19.
However, it could be bad news for people. It raises the possibility that the virus will pick up new mutations to help it adapt to its furry hosts, or even recombine with another rat virus. Either scenario could produce a novel pathogen that might spread to people and spark a new outbreak, the researchers warned.
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




