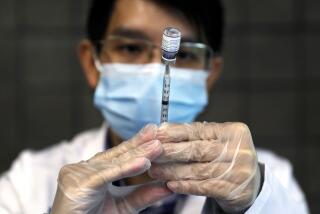
When your chance for a COVID-19 shot comes, don’t worry which one it is

- Share via
When getting a COVID-19 vaccine, there’s no sense being picky. You should take the first authorized vaccine that’s offered to you, experts say.
The newest COVID-19 vaccine on the horizon, from Johnson & Johnson, is probably a little less effective at preventing sickness than the two shots already being administered around the United States, made by Pfizer-BioNTech and Moderna. But it’s still worth getting.
On Friday, Johnson & Johnson announced that, in a 45,000-person trial, its vaccine was about 66% effective at preventing moderate to severe cases of COVID-19. No one who received the vaccine was hospitalized with or died of the disease, according to the company, which said it expected to seek emergency use authorization from the Food and Drug Administration as early as this week. If the FDA authorizes use of the vaccine, millions of doses could be shipped out of J&J’s warehouses beginning in late February.
The J&J vaccine is similar to the shots from Moderna and Pfizer-BioNTech but uses a different strategy for transporting genetic code into human cells to stimulate immunity to the coronavirus that causes COVID-19. The Pfizer-BioNTech and Moderna vaccines were found in trials last fall to be 94% to 95% effective at preventing the disease. They also prevented nearly all severe illnesses.
But the difference in those efficacy numbers may be deceptive. The vaccines were tested in different locations and at different phases of the pandemic. And J&J gave subjects in its trial only one dose of the vaccine, whereas Pfizer and Moderna have two-dose schedules, separated by 21 and 28 days, respectively.
The bottom line, however, is that all three do a good job at preventing serious illness.
“It’s a bit like, do you want a Lamborghini or a Chevy to get to work?” said Dr. Gregory Poland, director of the Mayo Clinic’s Vaccine Research Group. “Ultimately, I just need to get to work. If a Chevy is available, sign me up.”
So although expert panels may debate in the future about which vaccine is best for whom, “from a personal and public health perspective, the best advice for now is to get whatever you can as soon as you can get it, because the sooner we all get vaccinated, the better off we all are,” said Dr. Norman Hearst, a family doctor and epidemiologist at UC San Francisco.
Here are five reasons experts say you should take the J&J shot — assuming the FDA authorizes it — if it’s the one that’s offered to you first.
All three vaccines protect against hospitalization and death
Of the 10 people who had cases of severe disease in the Pfizer-BioNTech trial, nine had received a placebo, or fake, vaccine. Likewise, none of the 30 severe cases in the Moderna trial occurred in people who got the true vaccine.
Johnson & Johnson did not release specific numbers but said none of the vaccinated patients were hospitalized or died.
“The real goal is to keep people out of the hospital and the ICU and the morgue,” said Dr. Paul Offit, director of the Vaccine Education Center at Children’s Hospital of Philadelphia. “This vaccine will do that well.”
The efficacy levels could be a case of apples and oranges
The data that Pfizer-BioNTech and Moderna presented to the FDA for their vaccines came from large clinical trials that took place over the summer and early fall in the United States. At the time, none of the new coronavirus variants — some of which may be better at evading the immune responses produced by vaccines — were circulating here.
In contrast, the J&J trial began in September and was put into the arms of people in South America and South Africa as well as the United States.
Newly widespread variants in Brazil and South Africa appear somewhat better at evading the vaccine’s defenses, and it’s possible a new variant in California — where many J&J volunteers were enrolled — may also have that trait.
The J&J vaccine was 72% effective in preventing moderate to severe COVID-19 in the U.S. part of the trial, compared with 57% in South Africa, where a more contagious variant is the dominant strain. Another vaccine, made by the Maryland company Novavax, had 90% efficacy in a large British trial but only about 50% in South Africa.
Researchers once believed t would take months or even years for the virus to develop resistance to vaccines. The speedy evolution is largely a result of the virus’ unchecked spread.
The Pfizer-BioNTech and Moderna vaccines might not have gotten the same sparkling results had they been tested more recently — or in South Africa.
“This vaccine was tested in the pandemic here and now,” said Dr. Dan Barouch, a Harvard Medical School professor whose lab at the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center in Boston developed the J&J vaccine. “The pandemic is a much more complex pandemic than it was several months ago.”
Some of that difference in performance also could be attributable to different patient populations or disease conditions, and not just the proliferation of coronavirus variants. A large percentage of South Africans carry the human immunodeficiency virus, or HIV. Chinese vaccines have performed wildly differently in countries where they were tested in recent months.
“We don’t know which vaccines are the Lamborghinis,” Poland said, “because these aren’t true head-to-head comparisons.”
Speed is of the essence
To stop the spread of new and potentially more dangerous coronavirus variants and bring the pandemic to an end, we all need to be vaccinated as quickly as possible.
That means patients can’t be picky about which vaccine they accept, said Dr. Virginia Banks, a physician with Northeastern Ohio Infectious Disease Assn. in Youngstown. People “need to get vaccinated with the vaccines out today so we can get closer to herd immunity” to slow the spread of the virus.
The question of how many people must be vaccinated to reach herd immunity against COVID-19 is of crucial importance. Experts say the number is probably higher than previously thought.
Banks has worked hard to promote COVID-19 vaccines to skeptical minority communities, frequently appearing on local TV news and making at least two presentations by Zoom each week. To date, Black Americans have been vaccinated against COVID-19 at much lower rates than whites.
“There’s a downside to waiting,” said Dr. William Schaffner, a professor of preventive medicine and health policy at Vanderbilt University Medical Center. Delaying vaccination carries serious risks, given that more than 3,800 Americans have been dying every day of COVID-19.
The J&J vaccine appears to have some real advantages
First, it seems to cause fewer serious side effects, like the fever and malaise suffered by some Pfizer-BioNTech and Moderna vaccine recipients. High fever and dehydration are particular concerns in fragile elderly people who “have one foot on the banana peel,” said Dr. Kathryn Edwards, scientific director of the Vanderbilt Vaccine Research Program. The J&J vaccine “may be a better vaccine for the infirm.”
Many people may also prefer the J&J shot because “it’s one and done,” Schaffner said. It’s easier for administrators too: just one appointment to schedule.
The J&J vaccine is much easier to ship, store and administer
Although the Johnson & Johnson vaccine can be stored in regular refrigerators, the Pfizer-BioNTech vaccine must be kept long-term in “ultra-cold” freezers at temperatures between minus 112 degrees and minus 76 degrees Fahrenheit, according to the Centers for Disease Control and Prevention.
Both the Pfizer-BioNTech and Moderna vaccines must be used or discarded within six hours after the vial is opened. Vials of the J&J vaccine can be stored in a refrigerator and re-stored for later use if doses remain.
“Right now we have mass immunization clinics that are open but have no vaccine,” Offit said. “Here you have a single-dose regime with easy storage and handling.”
A person’s address — not their personal preference — may determine which vaccine they receive, said E. John Wherry, director of the Institute for Immunology at the University of Pennsylvania’s Perelman School of Medicine. He pointed out that the Johnson & Johnson vaccine was a simpler choice for rural areas.
“A vaccine doesn’t have to be 95% effective to be an incredible leap forward,” said Wherry. “When we get to the point where we have choices about which vaccine to give, it will be a luxury to have to struggle with that question.”
Arthur Allen and Liz Szabo write for Kaiser Health News, a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.