U.S. death toll tied to long COVID exceeds 3,500, CDC report says
The health challenges that a bout of COVID-19 sometimes leaves in its wake can be troublesome, scary and quite mysterious. New research confirms they can be deadly as well.
A study released Wednesday by the Centers for Disease Control and Prevention found that between January 2020 and June 2022, long COVID was implicated in at least 3,544 deaths in the United States alone.
For the record:
8:43 a.m. Dec. 14, 2022An earlier version of this headline said the country’s long COVID death toll exceeded 4,000; the toll exceeds 3,500.
The authors of the study acknowledge that their tally of long COVID fatalities is likely a significant undercount of people whose deaths were caused, at least in part, by COVID-19’s lingering effects. It represents a mere sliver — less than 0.4% — of the more than 1 million pandemic deaths that occurred during the study period in the United States.
But the new research contributes to mounting evidence that COVID-19’s toll doesn’t always end with a negative test. And it suggests that for many patients, new symptoms of poor health — from anxiety and sleep difficulties to heart arrhythmias and blood clots — may have unrecognized roots in a previous coronavirus infection.
Sometimes, those symptoms stem from infections patients didn’t even know they had.
“Viruses have long-term consequences,” said Dr. Ziyad Al-Aly, a physician with the Veterans Affairs St. Louis Health Care System who has studied the downstream health effects of an encounter with the SARS-CoV-2 virus.
“We’re pretty good at capturing acute disease,” he added. But researchers and medical professionals have a “major, major blind spot” when it comes to anticipating and detecting the longer-term fallout of a viral infection, he said.
Researchers are getting serious about understanding a disease patients call “long COVID.” Its symptoms include aches, fatigue, sleep problems and brain fog.
Al-Aly, who was not involved in the new CDC research, teaches epidemiology at Washington University in St. Louis. He led a recent study that detected sharp increases in 20 cardiovascular diagnoses in patients during the year that followed an infection with the virus that causes COVID.
The CDC report offers “a gross underestimate” of the deaths likely attributable to long COVID, Al-Aly said. But, he added, it makes clear that with more awareness and a better accounting system, researchers could begin to understand how often viral infections sow the seeds of future afflictions.
For much of the period covered by the new study, the lingering health effects of COVID-19 were not a well-defined syndrome. Scientists have come to know it as post-acute sequelae of COVID, or PASC, and the federal government launched a program to study it in February 2021.
In October 2021, the U.S. government created a unique medical code to identify PASC in medical records. But the cause of PASC’s wide-ranging symptoms frequently goes unrecognized, and U.S. doctors still don’t uniformly use the identifying medical code.
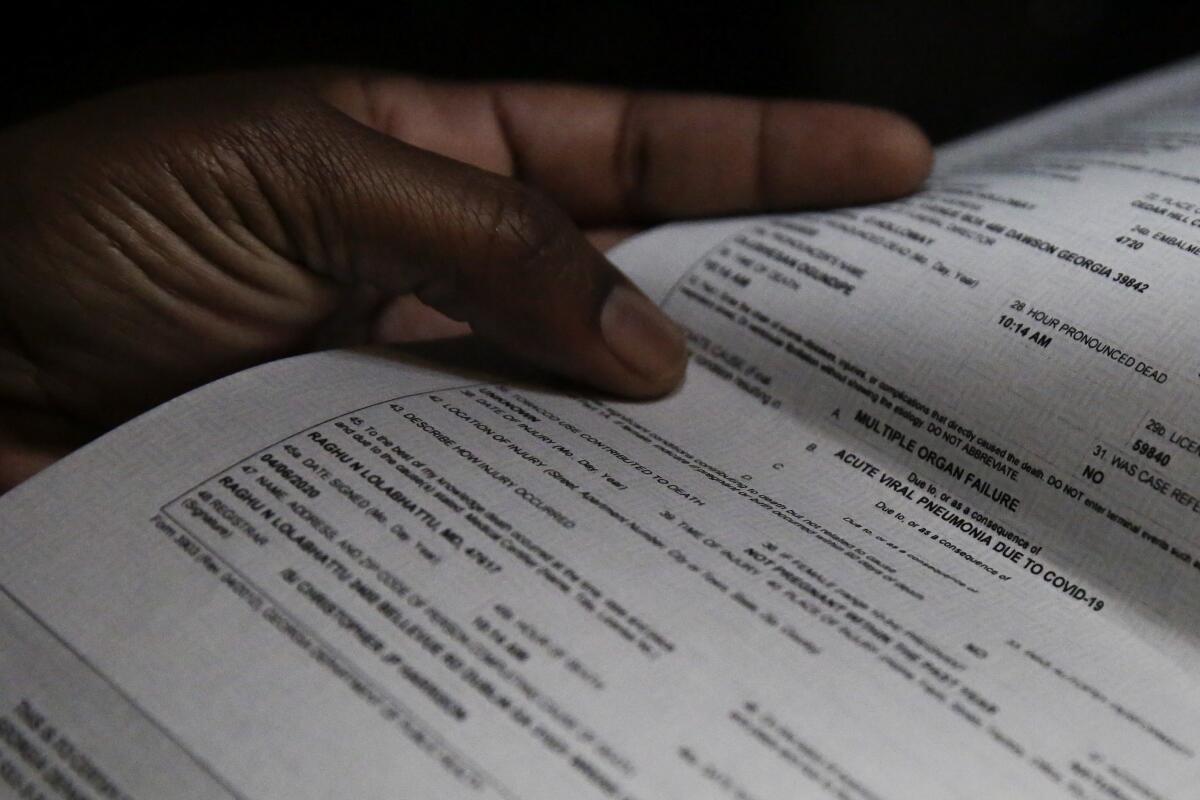
So to capture deaths in which PASC likely played a contributing role, researchers from the CDC’s National Center for Health Statistics had to hunt for clues buried in the language of death certificates. They started with 1,021,487 U.S. death certificates that indicated COVID-19 as the primary cause. Then they scanned each for references to “chronic COVID,” “long COVID,” “long-haul COVID” or “post-COVID syndrome” — all terms that have been widely used to describe the motley set of afflictions some patients experienced after they had apparently recovered from the disease.
In ‘The Long Haul,’ Ryan Prior recounts an unprecedented grass-roots effort to get the medical establishment to recognize a devastating shadow pandemic.
An exact description of PASC — which most medical professionals now refer to as long COVID — continues to evolve. Its hallmark symptoms are fatigue, cough, chest pain or shortness of breath, muscle weakness, brain fog, palpitations, and anxiety or depression.
The World Health Organization reports that about 1 in 4 people who have had COVID-19 continue to experience at least one symptom a month after diagnosis, and that roughly 1 in 10 have persistent symptoms after 12 weeks. In the United States, 7.5% of people who said they‘d had COVID-19 reported lingering effects three months after recovering.
Scientists are racing to understand long COVID’s cause. One surmise is that the syndrome is caused by residual viral debris that continues to activate and/or exhaust the immune system. Another attributes it to virus that hides and replicates undetected in organs where the immune system can’t get to it.
The simplest explanation — that a case of severe COVID-19 does lasting harm to organs — doesn’t account for why people who were scarcely ill sometimes wind up with long COVID.
The new research found that a post-infection spiral toward death was most readily detected in older people: Just over 78% of the death certificates that listed long COVID as a possible contributor were for patients 65 and older.
While women are thought to develop long COVID more frequently than men, the study found death certificates citing long COVID were slightly more likely to name men (51.5%) than women (48.5%).
A new research initiative will explore whether the persistence of coronavirus in the body plays a role in the development of long COVID.
Over the course of the pandemic, the list of organs that could be affected by COVID grew, yielding a picture of a virus that traveled well beyond the lungs and upper respiratory system. Likewise, long COVID may be found to affect an even wider range of organs as research proceeds.
Cardiovascular problems have already appeared on both expanded lists. Several months into the pandemic, doctors and scientists began to recognize that the coronavirus was causing blood clots, leading to strokes, heart attacks and emboli.
The study by Al-Aly and his colleagues showed that, in the period from one to 12 months after patients recovered from COVID-19, they had an increased risk for a wide range of cardiovascular problems.
Compared to a similar group of patients who had not had COVID-19, those who had were 52% more likely to suffer a stroke and 66% more likely to suffer some form of blockage in blood flow to the heart, including one that results in a heart attack. In addition, former COVID patients were 69% more likely than unaffected peers to develop some form of heart arrhythmia.
Not surprisingly, people who had been hospitalized with COVID were more likely to suffer cardiovascular complications. But even patients whose brush with the coronavirus was mild faced an elevated risk. And while those over 65 were most likely to develop these complications, younger and healthier patients saw their risks rise too.