The World Health Organization has issued a report that transforms how the world understands respiratory infections like COVID-19, influenza, and measles.
Motivated by grave missteps in the pandemic, the WHO convened about 50 experts in virology, epidemiology, aerosol science, and bioengineering, among other specialties, who spent two years poring over the evidence on how airborne viruses and bacteria spread.
However, the WHO report stops short of prescribing actions that governments, hospitals, and the public should take in response. It remains to be seen how the Centers for Disease Control and Prevention will act on this information in its own guidance for infection control in health care settings.
The WHO concluded that airborne transmission occurs as sick people exhale pathogens that remain suspended in the air, contained in tiny particles of saliva and mucus that are inhaled by others.
While it may seem obvious, and some researchers have pushed for this acknowledgment for more than a decade, an alternative dogma persisted — which kept health authorities from saying that COVID-19 was airborne for many months into the pandemic.
More than 200 researchers worldwide sign an open letter saying current guidance ignores evidence that the coronavirus readily spreads on microscopic particles known as aerosols that can hang in the air for long periods and float dozens of feet.
Specifically, they relied on a traditional notion that respiratory viruses spread mainly through droplets spewed out of an infected person’s nose or mouth. These droplets infect others by landing directly in their mouth, nose or eyes — or they get carried into these orifices on droplet-contaminated fingers.
Although these routes of transmission still happen, particularly among young children, experts have concluded that many respiratory infections spread as people simply breathe in virus-laden air.
“This is a complete U-turn,” said Dr. Julian Tang, a clinical virologist at the University of Leicester in the United Kingdom, who advised the WHO on the report. He also helped the agency create an online tool to assess the risk of airborne transmission indoors.
Peg Seminario, an occupational health and safety specialist in Bethesda, Md., welcomed the shift after years of resistance from health authorities.
“The dogma that droplets are a major mode of transmission is the ‘flat Earth’ position now,” she said. “Hurray! We are finally recognizing that the world is round.”
The change puts fresh emphasis on the need to improve ventilation indoors and stockpile quality face masks before the next airborne disease explodes. It is far from a remote possibility as measles is on the rise this year and the H5N1 bird flu is spreading among cattle in several states. Scientists worry that as the H5N1 virus spends more time in mammals, it could evolve to more easily infect people and spread among them through the air.

Traditional beliefs on droplet transmission help explain why the WHO and the CDC focused so acutely on hand-washing and surface-cleaning at the beginning of the pandemic.
Such advice overwhelmed recommendations for N95 masks that filter out most virus-laden particles suspended in the air. Employers denied many health care workers access to N95s, insisting that only those routinely working within feet of COVID-19 patients needed them. More than 3,600 health care workers died in the first year of the pandemic, many due to a lack of protection.
However, a committee advising the CDC appears poised to brush aside the updated science when it comes to its pending guidance on health care facilities.
Lisa Brosseau, an aerosol expert and a consultant at the Center for Infectious Disease Research and Policy in Minnesota, warns of a repeat of 2020 if that happens.
“The rubber hits the road when you make decisions on how to protect people,” Brosseau said. “Aerosol scientists may see this report as a big win because they think everything will now follow from the science. But that’s not how this works, and there are still major barriers.”
Scientists who have led the campaign to recognize the coronavirus as an airborne pathogen turn their attention to building design.
Money is one. If a respiratory disease spreads through inhalation, it means that people can lower their risk of infection indoors through sometimes costly methods to clean the air, such as mechanical ventilation and using air purifiers, and wearing N95 masks.
The CDC has so far been reluctant to press for such measures, as it updates foundational guidelines on curbing airborne infections in hospitals, nursing homes, prisons and other facilities that provide health care. This year, a committee advising the CDC released a draft guidance that differs significantly from the WHO report.
Whereas the WHO report doesn’t characterize airborne viruses and bacteria as traveling short distances or long, the CDC draft maintains those traditional categories. It prescribes looser-fitting surgical masks rather than N95s for pathogens that “spread predominantly over short distances.” Surgical masks block far fewer airborne virus particles than N95s, which cost roughly 10 times as much.
Researchers and healthcare workers have been outraged about the committee’s draft, filing letters and petitions to the CDC. They say it gets the science wrong and endangers health.
“A separation between short- and long-range distance is totally artificial,” Tang said.
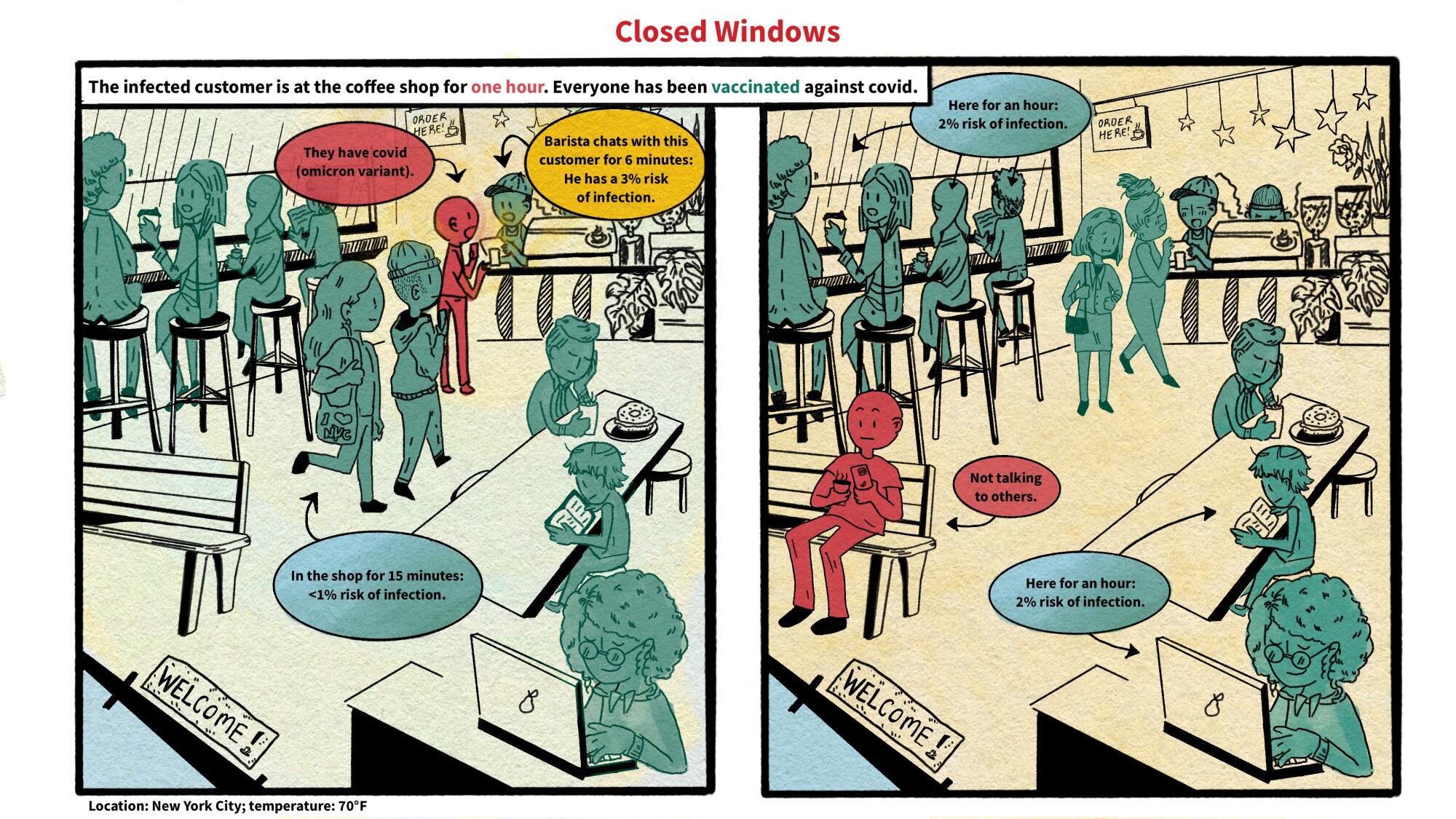
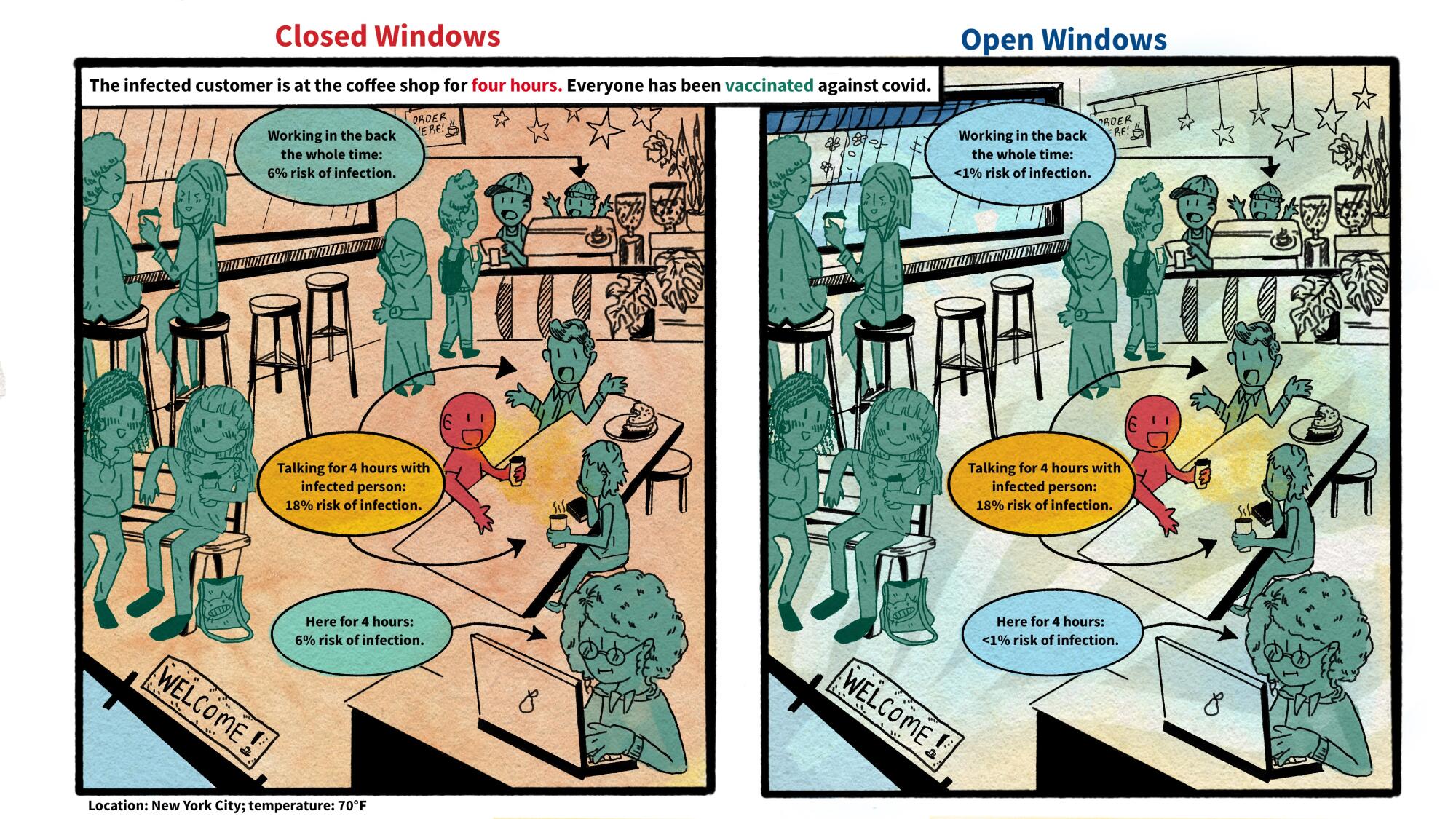
Airborne viruses travel much like cigarette smoke, he explained. The scent will be strongest beside a smoker, but those farther away will inhale more and more smoke if they remain in the room, especially when there’s no ventilation.
Likewise, people open windows when they burn toast so that smoke dissipates before filling the kitchen and setting off an alarm. “You think viruses stop after 3 feet and drop to the ground?” Tang said of the classical notion of distance. “That is absurd.”
The CDC’s advisory committee is composed primarily of infection control researchers at large hospital systems, while the WHO consulted a diverse group of scientists looking at many different types of studies.
For example, one analysis examined the puff clouds expelled by singers, and musicians playing clarinets, French horns, saxophones and trumpets. Another reviewed 16 investigations into COVID-19 outbreaks at restaurants, a gym, a food processing factory and other venues, finding that insufficient ventilation probably made them worse than they would otherwise be.
In response to the outcry, the CDC returned the draft to its committee for review, asking it to reconsider its advice. Meetings from an expanded working group have since been held privately. But the National Nurses United union obtained notes of the conversations through a public records request to the agency. The records suggest a push for more lax protection.
“It may be difficult as far as compliance is concerned to not have surgical masks as an option,” said one unidentified member, according to notes from the committee’s March 14 discussion. Another warned that “supply and compliance would be difficult.”
The nurses’ union wrote on its website, “The Work Group has prioritized employer costs and profits (often under the umbrella of ‘feasibility’ and ‘flexibility’) over robust protections.”
Jane Thomason, the union’s lead industrial hygienist, said the meeting records suggest the CDC group is working backward, molding its definitions of airborne transmission to fit the outcome it prefers.
Debates about the latest quarantine rules miss what matters most to fight COVID in 2024.
Tang expects resistance to the WHO report.
“Infection control people who have built their careers on this will object,” he said. “It takes a long time to change people’s way of thinking.”
The CDC declined to comment on how the WHO’s shift might influence its final policies on infection control in health facilities, which might not be completed this year.
Creating policies to protect people from inhaling airborne viruses is complicated by the number of factors that influence how they spread indoors, such as ventilation, temperature, and the size of the space.
Adding to the complexity, policymakers must weigh the toll of various ailments, ranging from COVID-19 to colds to tuberculosis, against the burden of protection. And tolls often depend on context, such as whether an outbreak happens in a school or a cancer ward.
“What is the level of mortality that people will accept without precautions?” Tang said. “That’s another question.”
KFF Health News, formerly known as Kaiser Health News, is a national newsroom that produces in-depth journalism about health issues.