Biden administration implores states to slow Medicaid cuts after 1 million lose coverage
- Share via
Too many Americans are losing Medicaid coverage because of red tape, and states should do more to make sure eligible people keep their health insurance, the Biden administration said Monday.
More than a million Americans have lost coverage through the program for low-income and disabled Americans in the past several weeks, following the end of pandemic protections on April 1, according to the latest Medicaid renewal data from more than 20 states.
After a three-year pause, most states have now resumed checking which Medicaid recipients remain eligible and dropping those who no longer qualify or don’t complete required paperwork. About 4 in 5 people dropped so far either never returned the paperwork or omitted required documents, federal and state data show.
Xavier Becerra, secretary of the Department of Health and Human Services, decried those numbers in a letter sent to state governors on Monday.
“I am deeply concerned with the number of people unnecessarily losing coverage, especially those who appear to have lost coverage for avoidable reasons that State Medicaid offices have the power to prevent or mitigate,” he wrote.
California will soon require Medi-Cal recipients to prove their eligibility again. But it has a safety net for people who lose their coverage.
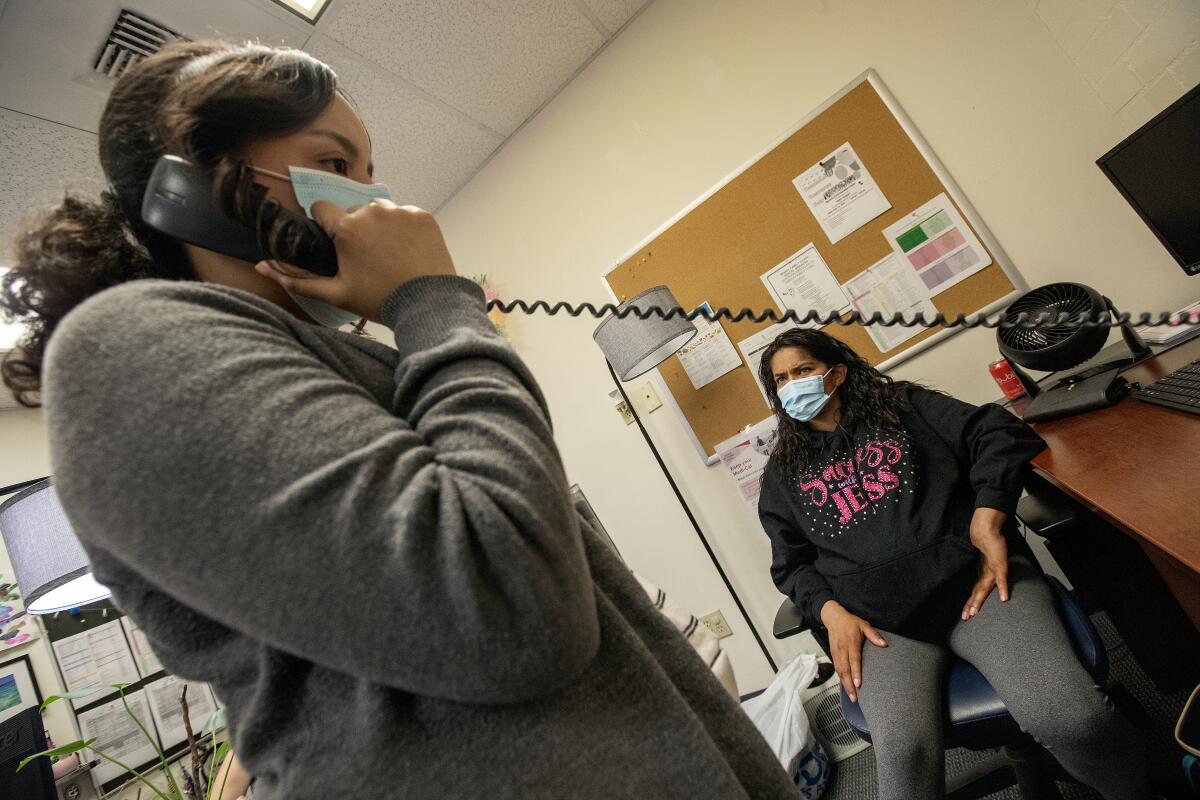
The Biden administration outlined several optional steps states can take to ensure everyone who still qualifies for the safety-net health insurance program stays covered. For instance, states can pause the cancellations to allow more time to reach people who haven’t responded. Health insurance companies that manage Medicaid plans can help their enrollees fill out the paperwork.
Some states were already choosing to take extra time. Though Wyoming began renewals in May, the state is being “deliberately cautious” and won’t drop people for incomplete paperwork until July or August, state Health Department spokesperson Kim Deti said. Oregon won’t start those cancellations until October.
Officials in other states have demonstrated no eagerness to slow the cuts.
About 10% of Arkansas’ Medicaid and Children’s Health Insurance Program enrollees have already been dropped, nearly all because they didn’t complete paperwork. Arkansas is speeding through the redeterminations in just six months, while most other states are taking about a year, as HHS recommended. Despite outcry from some federal lawmakers and advocates, Medicaid officials in the state wrote on June 8 that they would continue to “swiftly disenroll” people who no longer qualify.
That could be disastrous, said Joan Alker, executive director of Georgetown University’s Center for Children and Families.
“My big worry is that we could lose millions of families quickly,” she said. “It’s going to be very hard to get them back.”
California is weighing new continuous-enrollment policies for children up to age 5 who rely on Medicaid. They’d keep their coverage even if their household income changes.
Becerra also wrote that he is “particularly concerned” about children losing coverage, although the administration doesn’t know exactly how many kids have been dropped. States don’t have to report numbers by age to federal authorities, said Dan Tsai, director of the Center for Medicaid and CHIP Services.
Tens of thousands of kids are losing coverage, according to data from states that shared it. In Indiana, of the 53,000 dropped in the first month, one-third were kids. In South Dakota, more than half were kids. In Arkansas, nearly 55,000 kids were dropped in the first two months.
Becerra also urged governors to work more directly with families at risk of losing coverage. State agencies should team up with schools, faith-based groups, pharmacies, and other community organizations to help enrollees better understand how to stay on Medicaid, he wrote.
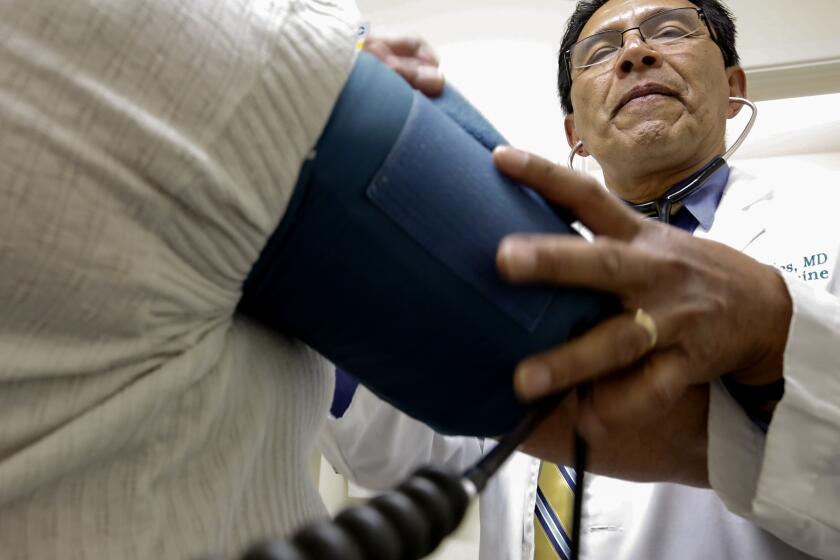
As the federal government has rolled back rules that helped people hang on to Medicaid during the COVID-19 pandemic, health providers fear the fallout could be disastrous for patients
In most states, people who still qualify for Medicaid but lose coverage because of state errors or incomplete paperwork have 90 days to ask for their coverage back.
Some officials view the large number of paperwork-related cancellations as no big deal because people can reapply if they still qualify. But it’s not that simple, Alker said. Many people don’t know their appeal rights, and the grace period doesn’t apply to all adults in several of the hardest-hit states.
Alker said states will temporarily save money from not having to pay for enrollees’ care. But in the meantime, people won’t be able to afford their regular medications. Some will end up in the emergency room sicker than before, she said. “There’s really nothing good that comes out of these gaps in coverage.”
This article was produced by KFF Health News, formerly known as Kaiser Health News, a national newsroom that produces in-depth journalism about health issues.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.