Column: Stop fretting about ‘herd immunity’ — we may already be there

As if to assuage an insatiable public appetite for bad news, every advance in the fight against COVID-19 seems to inspire a surge in pessimistic prophecies.
The latest example involves the prospects of reaching “herd immunity” — that is, a level of vaccinations and natural recoveries that will render the virus no longer a threat to public health.
A number of recent reports cast doubt on whether that goal is reachable. A New York Times article conjectured that herd immunity is “not attainable — at least not in the foreseeable future, and perhaps not ever.”
Trying to reach ‘herd immunity’ as if suddenly there’s going to be this magic day when...the virus is completely gone—that’s probably a fantasy. But getting the virus to a tolerable level where we don’t have to alter our way of life is probably very achievable.
— David Dowdy, Johns Hopkins
The article placed the blame partially on “vaccine hesitancy” leaving too many Americans unimmunized. The harvest was a surge of Twitter-based obloquy directed at Americans who turn down a COVID-19 vaccine.
Yet respected immunologists say the concept of herd immunity is widely misunderstood — and in fact the conditions for its attainment in the U.S. may be close or already have been reached.
That’s because the level of vaccination in much of the country already has been sufficient to drive the levels of infection steadily lower and foster a consistent reduction in new cases.
Get the latest from Michael Hiltzik
Commentary on economics and more from a Pulitzer Prize winner.
You may occasionally receive promotional content from the Los Angeles Times.
Indeed, the daily average of new cases per capita, compiled by the Washington Post, has fallen over the last seven days in all but five states. In two of the five, Wyoming and Maine, the figure rose by only 1% and in a third, New Mexico, it was flat.
What’s causing confusion, experts say, is that laypersons tend to equate herd immunity with the complete eradication of the virus.
“That’s not what infectious disease doctors mean by ‘herd immunity,’” says Dr. Monica Gandhi, a professor of medicine at UC San Francisco. “Unfortunately, we’ve only eradicated a single virus in the history of mankind, and that is smallpox.”
Gandhi adds, “We live very comfortably with other viruses for which we’ve achieved herd immunity, it’s just that the public doesn’t know it.”
For example, few Americans devote much attention to measles, a highly infectious disease, because childhood inoculations are so effective. That’s also true of polio, which lost its capacity to terrorize the public soon after mass inoculations with the Salk vaccine were launched in the mid-1950s.
Polio is now regarded as having been eliminated in the Western Hemisphere, though outbreaks still occur in less developed regions.
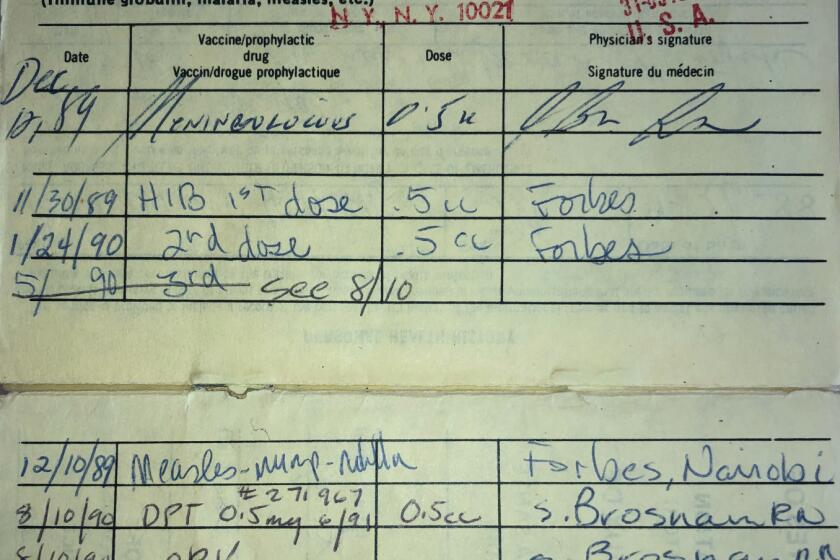
The idea of vaccine passports isn’t new, as international travelers and families with school-age children will tell you.
Vaccinations and immunity achieved naturally by those who have had COVID-19 drive down the transmission of the virus to the point where exposure is rare.
“The non-immune are protected by not seeing the virus,” Gandhi told me. “It’s just not circulating at high rates. It will keep on going down and down in the population.”
That effect is already being seen in communities that have reached a high rate of vaccinations.
They include Britain, where more than 65% of all residents have received at least one dose of a COVID-19 vaccine; Israel, where 57% of the population is fully vaccinated, and San Francisco, where 74% of residents over 16 have received at least one dose and 56% a full dose. In all three locations, case rates are plummeting.
In other countries, notably India, the virus is still out of control — but the experience of locations where vaccination campaigns have been strong suggests paths for success to places currently beleaguered by COVID-19.
For epidemiologists, that’s a very hopeful sign.
“The idea of trying to reach ‘herd immunity’ as if suddenly there’s going to be this magic day when we can all go back to normal and the virus is completely gone — that’s probably a fantasy,” says Dr. David Dowdy, an epidemiologist at Johns Hopkins Bloomberg School of Public Health.
“But getting the virus to a tolerable level where we don’t have to alter our way of life is probably very achievable,” he says. “We’re already at a stage in the U.S. where we’re seeing case counts go down.”
Credit for that result belongs to the remarkable efficacy of the vaccines. The two-dose vaccines produced by Moderna and the Pfizer-BioNtech vaccines, which are based on similar technologies, are about 95% effective at protecting against severe disease.
The third widely used vaccine, a one-dose preparation produced by Johnson & Johnson, has been shown to be 66% effective overall and 85% effective at protecting against severe COVID-19.
“That doesn’t mean that we can’t still have outbreaks, or that if we have variants to which the vaccines are less effective we can’t have a resurgence, or if people suddenly go back to normal by having big indoor gatherings again that we couldn’t start to see cases go up again,” Dowdy says.
Dowdy points out that the toll from the pandemic and its impact on daily life was so monumental that fear of the disease may linger, affecting our lifestyles out of proportion to the level of threat. But he doesn’t expect a new wave of infections anywhere near the scale of those that swept across the country last summer and at the end of last year.
“People’s perception of the endgame is what’s off,” Dowdy says. “We’re going to have this low level of COVID for a long, long time, and the question is how are people going to react to that. The answers to that are not going to be epidemiological, but social, political and behavioral.”
Pfizer and Moderna will rake in the big bucks from their COVID vaccines. That’s a sign of a broken system.
He’s right about that. A good example was an April 17 exchange between Rep. Jim Jordan (R-Ohio) and Dr. Anthony Fauci, the respected government infectious disease expert, at a House committee hearing.
“Are we just going to continue this forever?” Jordan asked, referring to mask and social distancing rules. “What objective outcomes do we reach before Americans get their liberty and freedoms back?”
Leaving aside that Jordan spoke as though Fauci were to blame for imposing stringent measures on Americans’ lifestyles — in fact, those decisions are in the hands of local political officials — his demand for a certain date or specific statistic that would warrant the immediate lifting of all anti-COVID-19 mandates was scientifically out of place.
Fauci tried patiently to set him right, without success. “You’re indicating ‘liberty and freedom,’” he replied. “I look at it as a public health measure to keep people from dying... This will end, for sure, when we get the level of infection very low.”
Some debate the precise percentage point of inoculation in the U.S. population that will trigger herd immunity. Getting hung up on that particular number isn’t a worthwhile exercise.
Simply stated, the higher the percentage of people who have been vaccinated, the faster transmission will fall. New cases will decline even before the population reaches full herd immunity — as has been happening.
Doubts about the battle against COVID-19 may linger. Gandhi believes that worries about how long immunity will last may also be misplaced. That can have global consequences, for the desire to maintain supplies of booster shots could keep vaccines from being distributed in quantity to parts of the world where they’re desperately needed now.
So how will we know when we can declare victory? For Gandhi, that will be the point at which case statistics cease to be the focus of public obsession or are reported daily in newspapers or on cable.
The impulse to test even asymptomatic patients will ebb, and the cases that do arise will be managed by the healthcare system as routinely as measles or mumps.
We may not be there yet, but to epidemiologists examining the trend of new cases, we may not be too far off.
More to Read
Get the latest from Michael Hiltzik
Commentary on economics and more from a Pulitzer Prize winner.
You may occasionally receive promotional content from the Los Angeles Times.