What Californians should do now to prepare for a possible spring Omicron BA.2 surge

Is California doing enough to prepare for a potential increase in cases of the Omicron subvariant BA.2 this spring?
California has made great strides in improving access to vaccinations and testing, but officials say there’s plenty of room for improvement, and that doing so is essential, given concerning trends elsewhere in the country, especially in the Northeast.
Early signals
The Omicron subvariant BA.2 — about 30% to 60% more transmissible than the currently dominant Omicron subvariant — is being detected more frequently, according to the U.S. Centers for Disease Control and Prevention. And, even though the weekly count of new coronavirus cases nationally has been declining or flat, there are some hints that they may be starting to rise in New York City.
In California, sewage treatment sites serving six counties are reporting at least a doubling of detected coronavirus samples in wastewater over the last 15 days. The sites serve San Diego, Contra Costa, Fresno, Monterey, Santa Cruz and San Benito counties, according to the CDC’s wastewater tracker as of Tuesday morning.
Los Angeles County isn’t seeing as high of a percentage of BA.2 cases as places like New York and Chicago, but the L.A. County Department of Public Health is saying nationwide trends suggest that Angelenos “should be prepared to mitigate the risk of increased transmission associated with this more infectious subvariant.”
“The increasing presence of the highly transmissible BA.2 subvariant in many regions of this country reminds us that we need to remain vigilant and prepared for the possibility of more cases in the near future,” L.A. County Public Health Director Barbara Ferrer said in a statement Monday.
“And while discouraging to face this possibility, the best way to blunt another surge in cases from increasing hospitalizations and deaths is to increase vaccination and booster coverage,” Ferrer said. “Waiting until we start seeing increases in cases is not optimal, since once there are more people testing positive, there is already more community transmission.”
With infections rising in parts of Africa, Asia and Europe, officials say they wouldn’t be surprised if new cases climbed again in the U.S.
Booster shots
Officials have been concerned about lackluster rates of booster shots, which help further protect vaccinated people — especially older people and those with underlying health concerns — from severe illness, hospitalization and death. While 71% of L.A. County’s 10.1 million residents are considered fully vaccinated, only 36% have received a booster dose.
Even among the county’s highly vaccinated senior population, booster rates are not ideal. About 90% of L.A. County’s 1.4 million seniors age 65 and up are considered fully vaccinated. But only 63% of those 1.4 million have received a booster shot.
It’s important to get a booster shot, experts say.
According to data published by the CDC in February, when Omicron was dominant, vaccine effectiveness against hospitalization was 71% during the first two months after people completed their primary two-dose vaccination series of the Pfizer-BioNTech or Moderna shots. But that fell to 54% five months after the second dose. A booster shot brought vaccine effectiveness against hospitalization to 91% in the first two months following the injection, and was at 78% four months after that shot.
During a time Omicron was dominant, vaccine effectiveness against death or needing a mechanical ventilator to breathe was 79% for people who received two vaccination doses, and 94% among those who received a third shot, according to data published this month by the CDC.
It’s uncertain whether an increase in coronavirus cases fueled by BA.2 could result in merely a ripple or the kind of rapid surge that would strain hospital systems. Experts have suggested reasons for why a BA.2 wave in the U.S. could end up being either mild or quite worrisome.
Masking up even as rules ease
The unsettled outlook is a big reason why California health officials still strongly recommend universal wearing of masks in indoor public settings.
There are a number of reasons why some health officials express some concern about preparing for the next surge.
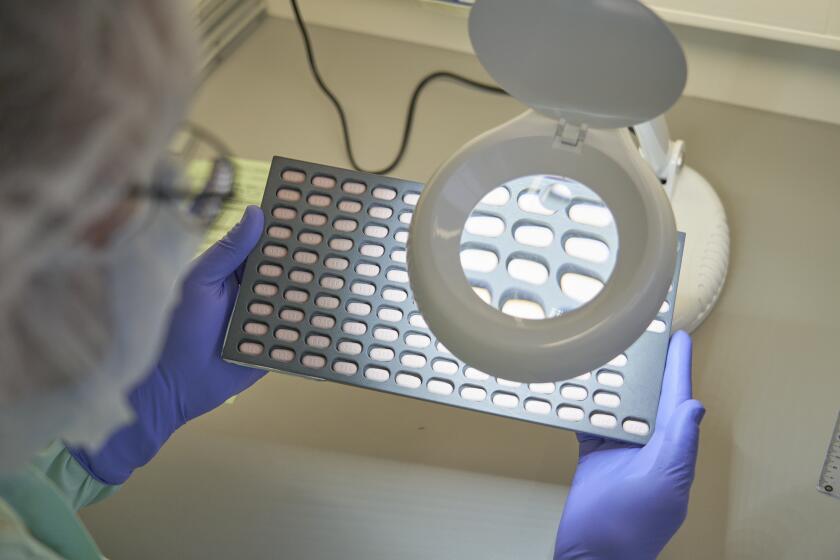
A drug option
In Los Angeles County, more needs to be done to improve access to anti-COVID drugs, like Paxlovid pills that are intended for newly diagnosed coronavirus-positive patients at higher risk for severe COVID-19, Ferrer said. Drugs like Paxlovid must be given within a certain number of days after symptoms begin, or from the day of a positive coronavirus test, and they work best if given early.
L.A. County has launched a program that offers anti-COVID pills for free to infected people who get tested, or show test results, at select pharmacies.
There were 116 sites in L.A. County in the most vulnerable communities that were dispensing anti-COVID drugs as of last week; Ferrer said getting that number to at least 150 would be adequate, with an ultimate goal of establishing at least 250 sites in these areas.
Some officials have expressed concern that anti-COVID drugs are sitting unused because the populace doesn’t know about them.
In remarks to the California Medical Assn. on March 8, State Epidemiologist Dr. Erica Pan suggested that lack of familiarity with the potentially lifesaving anti-COVID medications are a reason the drugs are being “turned away at the local level.”
Pan told doctors that we “need to kind of increase awareness — that if you have patients that are testing positive, that are risk for hospitalization, they really should seek treatment.”
L.A. County has launched the “test to treat” COVID-19 program announced by President Biden in his State of the Union address March 1, which offers anti-COVID pills for free to newly infected people who get tested, or show their test results, at select pharmacies with on-site clinics. A list is available on the county’s website or by calling (833) 540-0473.
Ferrer is also seeking to increase the overall percentage of residents age 12 and up in the most vulnerable communities that have received a booster shot. Currently, only 36% of them have received a booster shot; Ferrer’s immediate goal is to get that figure to at least 45%, and ultimately past 60%.
California health authorities have continued to say that COVID-19 still remains a more potent public health threat than the flu, and that it’s important that people get their shots — especially seniors who haven’t received their booster and children age 5 to 11 who have been vaccinated at lackluster rates.
In Los Angeles County, only 30% of children 5 to 11 are considered fully vaccinated — the lowest figure for any age group. By comparison, 85% of adolescents age 12 to 17 are fully vaccinated in L.A. County.
The low vaccination rates among young children are a concern. There were 66 COVID-related deaths nationally among children 5 to 11 in the year that ended Oct. 2, according to CDC data, making COVID-19 equivalent to the eighth-leading cause of death in that age group when compared to data of deaths from 2019.
According to the CDC, since the start of the pandemic, 167 COVID-19 deaths have been reported nationally in children 5 to 11.
Racial disparities
Officials are also concerned about racial and ethnic disparities in vaccinations. In L.A. County, 55% of Black and 57% of Latino residents are considered fully vaccinated, compared to 73% of white and 82% of Asian American residents.
“A lot of people talk about: Are we at an endemic phase yet?” Pan said. Bringing the pandemic to an endemic state means that COVID-19 is no longer affecting hospitals significantly and is no longer generally disruptive to daily life.
But we’re not there, Pan said. In California since October, there have been more than 10 pediatric COVID-19 deaths, already greater than the total number of pediatric deaths from the flu in the 2016-17 flu season, according to data she shared.
In addition, the total weekly number of deaths from all causes in California has recently still remained above pre-pandemic highs, with COVID-19 still a major factor.
This past winter, California recorded nearly 8,000 deaths from all causes during its worst week, with COVID-19 blamed for nearly 25% of them.
Over the past five years, this number was only exceeded by the previous winter’s COVID-19 surge. During that winter’s worst week, 12,000 deaths from all causes were recorded, with 45% of them blamed on COVID-19.
Both peaks were worse than at any point during the three years preceding the pandemic. The previous high number of weekly deaths from all causes was about 7,000 in the winter of 2017-18, with flu causing fewer than 5% of fatalities, even though there was a very bad flu season under way at that time, Pan said.
“So this means we are not at a stage where this [COVID-19 pandemic] is, you know, endemic or normalized yet,” Pan said. “We are not at a place yet where this is just like the flu.”
L.A. County is in good shape in other aspects, with plenty of vaccination sites — more than 1,100 at fixed locations and about 800 mobile vaccination sites, Ferrer said. Testing access is good — the average wait time to get a test at county-run testing sites is just 10 minutes, Ferrer added.
Ferrer has reiterated that coronavirus case rates in L.A. County for much of this month have remained at substantial levels, and haven’t reached moderate levels, in which risk of infection would be lower.
Testing
Ferrer encouraged people to get tested if they have symptoms of COVID-19, have been in close contact with someone who has tested positive, before and after travel, and prior to indoor visits at nursing homes.
She also encouraged people to take rapid tests just before or after events and gatherings, especially for people who are either at higher risk for COVID-19, live with someone at higher risk, or are meeting with someone at higher risk. Testing is free at sites listed on the county’s website.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.