As if COVID-19, inflation and the economy weren’t enough, the rise in monkeypox cases has given Californians yet another thing to worry about.
The disease — characterized by a rash and lesions that can look like pimples, bumps or blisters — primarily spreads through prolonged skin-to-skin contact with those lesions, which may be in hard-to-see places on the body or be mistaken for some other skin issue. Although rarely fatal, the disease can be quite painful.
Update:
6:19 p.m. Aug. 22, 2022 This story has been updated to include expanded eligibility information from the Los Angeles County Department of Public Health.
Monkeypox has gained a foothold among men and transgender people in the LGBTQ community in Los Angeles. The Los Angeles County Department of Public Health has received a limited number of doses of monkeypox vaccine from the federal government, and is offering them only to people currently deemed at risk.
Right now, monkeypox cases are “approaching an exponential curve ,” said Dr. Peter Chin-Hong, an infectious-disease expert at UC San Francisco. Nevertheless, for people outside the affected communities, the risk of catching monkeypox seems to be low at the moment. And if current vaccination efforts are successful, we may be able to wipe out monkeypox. But if it spreads to animals, the disease could become endemic in the United States.
How does monkeypox spread? How dangerous is it? How contagious is it? Can infected people with no symptoms pass on the disease to others? Can it be spread through the air? Who can get a vaccine? What can people do after they’re fully vaccinated? What should people do to avoid getting monkeypox?
You have questions. We asked experts for answers.
Have more inquiries about monkeypox? Send us an email at utility@latimes.com .
Who's eligible for a monkeypox vaccine in L.A. County? Anyone of any gender identity or sexual orientation is eligible to receive a monkeypox vaccine in L.A. County if they have had sex in exchange for money, food, shelter, or other goods or needs in the past 14 days.
You’ve had multiple or anonymous sex partners in the last 14 days. You’ve had skin-to-skin or intimate contact (such as kissing or hugging) with people at large venues or events in the past 14 days. You are on HIV PrEP medication. You’ve had anonymous sex or sex with multiple people within the last 21 days at a commercial sex venue or similar location. (Ward Carpenter, director of health services for the Los Angeles LGBT Center , said that would include such places as a sex party; a club, sauna or spa where people tend to engage in sexual activities; or an establishment where people pay money to gain entry and have sex.) You’ve had high or intermediate exposure to monkeypox (the CDC has a list of what qualifies as exposure at those levels). You’ve attended an event or venue where there was a high risk of exposure via skin-to-skin or sexual contact with people who have monkeypox. You are experiencing homelessness and engaging in high-risk behaviors. You’ve had gonorrhea or early-stage syphilis in the last 12 months. You are in jail and have been identified as high-risk by clinical staff. You are severely immunocompromised — for instance, you are undergoing chemotherapy, are on high-dose steroids or other immunosuppressants, or have advanced or uncontrolled HIV. The monkeypox vaccine is now available to minors. Those who are 16 or 17 years old will need to either be accompanied by a parent or legal guardian or bring a consent form signed by one. Children 15 and younger must be accompanied by a parent, a legal guardian, or by a responsible adult who has a consent form signed by the child’s parent or guardian.
Eligibility criteria may change. The public health department’s website maintains
a list of the latest eligibility information .
How do I get a monkeypox vaccine if I'm eligible? To get the monkeypox vaccination in Los Angeles County, you need to sign up through the public health department. When vaccine appointments are available, the department lets you pre-register for an appointment at a clinic . When you pre-register, you’ll need to enter your name, phone number and email address and answer some questions. The confirmation notice says it will place you on a list, and you’ll be notified when it’s your turn to get vaccinated.the top of this page on the department’s website. Enter your email address in the box and click “submit.”
What do I do if I think I have monkeypox or have been exposed to it? If you think you have been exposed to or have monkeypox, do not go to a vaccination site. Contact your healthcare provider, call the L.A. County information line at 2-1-1, or visit a public sexual health clinic . You can also call the L.A. County Public Health Department call center at (833) 540-0473 (staffed daily from 8 a.m. to 8:30 p.m.) with monkeypox questions and concerns.
What are the early symptoms of monkeypox? Symptoms of monkeypox typically begin within five to 21 days of exposure. Early indicators include flu-like symptoms such as fever, malaise, chills, muscle aches and swollen lymph nodes, followed by a rash and the telltale monkeypox lesions. The department of public health has photos of what the blisters look like and more information on monkeypox symptoms .
How dangerous is monkeypox? Monkeypox is rarely fatal, and there have been no deaths in the United States from monkeypox during this outbreak. Globally, as of Aug. 11, there have been 31,665 cases of monkeypox and 12 deaths from it since May 2022, according to data from the World Health Organization . Though symptoms are usually mild, 36 people have been hospitalized for monkeypox as of Aug. 11 in California.
Can only gay or bisexual men get monkeypox? No. While the outbreak is spreading primarily among gay and bisexual men, as well as some transgender and nonbinary people, anyone — regardless of gender or sexual orientation — can become infected.Department of Public Health . (2% of respondents in that group identified as straight or heterosexual, and for 14%, their sexual orientation was unknown.) State and national health officials have reported the same demographic trends, and for that reason, gay and bisexual men, as well as some other queer people, remain most at risk.
How does monkeypox spread? “Its most efficient route of transmission is close, prolonged, skin-to-skin contact,” said Anne Rimoin, a professor of epidemiology at the UCLA Fielding School of Public Health and a member of the World Health Organization’s emergency committee on monkeypox. While the virus is capable of spreading via respiratory secretions and surface transmission on contaminated objects, “ that’s not what we are seeing as the primary mode of transmission in this outbreak. What we’re seeing is the vast majority of cases are from prolonged skin-to-skin contact, generally in the context of sex,” she said.
When will you know if you have monkeypox if you've been exposed, and how long does the infection last? Symptoms can appear as early as five days after exposure. Dr. Leo Moore, director of clinical services for the Los Angeles County Department of Public Health, said people typically develop symptoms a week or two after being exposed, though it can take as long as three weeks for symptoms to appear.
Can monkeypox spread asymptomatically? “It does not, at this point, look like there’s risk from asymptomatic spread,” said Dr. Jay Gladstein, chief medical officer for APLA Health, an L.A. group focused on providing healthcare to the LGBTQ community.
Is monkeypox considered an STD? Not exactly. In this outbreak, monkeypox is spreading through prolonged skin-to-skin contact and shared clothing and bedding. Experts believe the current outbreak in North America and Europe likely started with people having sex at raves in Spain and Belgium. But it’s not a disease that specifically spreads through bodily fluids, like chlamydia or gonorrhea, and using a condom won’t prevent it from spreading.issued a safety warning about monkeypox noting that dancing and sex-adjacent activities including kissing could also be vectors for infection.
What can I do after I get my monkeypox vaccine? That’s unclear. You are not fully vaccinated until two weeks after your second dose. And right now, L.A. County is prioritizing getting first doses into arms over scheduling second shots. World Health Organization’s emergency committee on monkeypox. “That’s not to say it won’t work, we just don’t have enough data to make definitive statements.”Los Angeles LGBT Center . “In a month or two, we’ll have a lot better idea on how well this is working to keep people safe.”
How does the state of emergency change things? The state of emergency proclamation issued Aug. 1 makes it easier for the state to coordinate its monkeypox outbreak response by ordering all state agencies to follow directions from the Office of Emergency Services and the California Department of Public Health. The order also allows EMS workers to administer vaccines.Los Angeles LGBT Center . “We’re limited by the (vaccine) supply and also the sheer human capacity to handle this.”
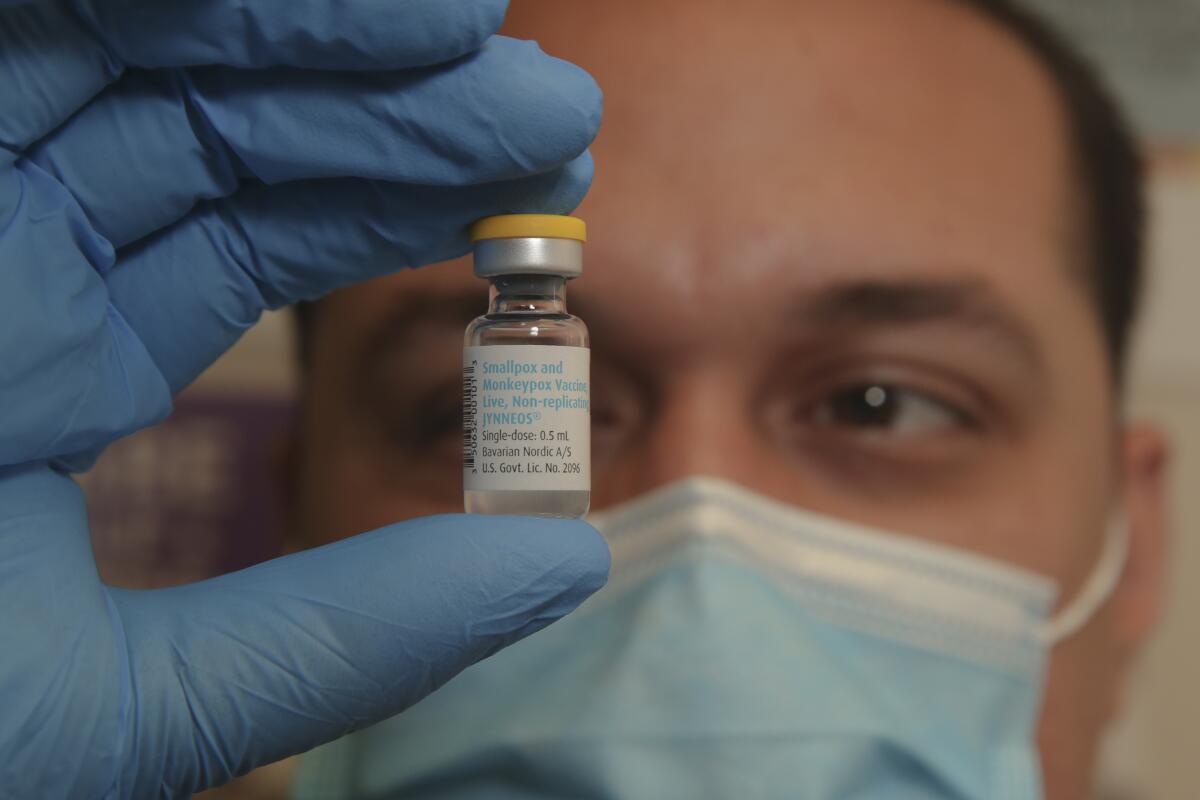
What if I already got the smallpox vaccine? The last routine shots for smallpox were given in the 1970s in the U.S. Georges Benjamin, executive director of the American Public Health Assn., said you would probably have some degree of protection from monkeypox if you got the smallpox shot pre-1980, but you should still get the Jynneos vaccine if you’re exposed or are otherwise eligible.
What do I need to do to avoid monkeypox? If you are not a member of the currently affected community — gay and bisexual men and transgender people — experts say you don’t need to change anything about your behavior right now. justifiably controversial . Ward Carpenter, director of health services for the Los Angeles LGBT Center , said he recommends people consider moderating their own behavior in a way that’s workable for their lifestyle.
Will everyone have to get vaccinated for monkeypox eventually? Right now, it doesn’t seem like that will be necessary, said Anne Rimoin , a professor of epidemiology at the UCLA Fielding School of Public Health and a member of the World Health Organization’s emergency committee on monkeypox.
With additional reporting by Rong-Gong Lin II, Luke Money, Taryn Luna and Melody Gutierrez.
About The Times Utility Journalism Team
This article is from The Times’ Utility Journalism Team. Our mission is to be essential to the lives of Southern Californians by publishing information that solves problems, answers questions and helps with decision making . We serve audiences in and around Los Angeles — including current Times subscribers and diverse communities that haven’t historically had their needs met by our coverage.Jon Healey , Ada Tseng , Jessica Roy and Karen Garcia .