
HUNTINGTON, W.Va. — Signs advertising drug rehab or access to emergency overdose kits are easy to spot here. It’s harder to find the downtown homeless encampment, a discrete cluster of three tents along the Ohio River, squeezed by a bridge and a construction site.
To people who believe drug addiction is to blame for the mushrooming tent cities in Los Angeles, San Francisco and Portland, Ore., West Virginia presents a paradox. It leads the nation in overdose deaths per capita — by a wide margin. But this state best known for coal mines and the leafy Appalachian Mountains has one of the country’s lowest rates of homelessness.

“People conflate these crises,” said Dr. Margot Kushel, a UC San Francisco professor who led the largest representative study of homeless people in three decades, released earlier this year. “They are related but they are far from one and the same.”

Huntington, a college town and riverside port city along the border of Ohio and Kentucky that was once dubbed the overdose capital of America, illustrates the knotty relationship between the two plagues.
Nearly two-thirds of the homeless people here self-reported that they were struggling with addiction this year. But cheap and available housing has kept the official homeless count at 244 people in Huntington’s two-county service area, up since the beginning of the COVID-19 pandemic but still about a fourth of the per capita homeless population of Los Angeles County.

Housing markets operate a bit like rock concerts. Almost everyone can get in when demand and prices are low. But when Taylor Swift comes to town, and far more people want a seat than can get one, the barriers to entry grow, even for the cheapest tickets.
Those with the most hurdles — addiction, mental illness, criminal convictions and poverty, in the case of housing — are most likely to be stuck at the end of the line and shut out of a tight market.
From there, the problems feed off each other. People who lose housing are more likely to increase their drug and alcohol use, according to research by Kushel and others. And experiencing both homelessness and drug addiction — along with mental health issues in many cases — lengthens the time it takes to tackle each of the problems.
“A lot of people don’t understand that — but my substance use was kind of fleeting,” said Amanda Leffler, a 42-year-old Huntington resident who was homeless for about 15 years after leaving her husband.
1

2

3

1. Amanda Leffler said she kicked her drug habit before she found a subsidized apartment seven years ago, but she still has trouble living inside. 2. Amanda Leffler cleans her apartment. 3. Amanda Leffler stands in front of the apartment.
(Jason Armond/Los Angeles Times)
She began taking more prescription drugs after getting hit by a paint truck, but shame from being homeless pushed her over the top, she said.
“The amount of loathing that you can sense, just by somebody looking at you from across the street, is enough to break your damn soul,” Leffler said. “So if you can imagine having that happen for 24 hours a day, every day, for years and years and years, you’d get f—ing high too.”
Using drugs made it harder for her to imagine a life off the street, where she would need to shop and cook or perform tasks beyond “basic survival instincts,” she said.
Leffler said she kicked her drug habit before she found a subsidized apartment seven years ago, but she still has trouble living inside.
Leffler is a patient at OVP, a primary care and outpatient treatment clinic where signs under the fluorescent lights tell patients that they are loved and that “you can start where you are and change the ending.”
Changing the ending is hard work when it involves OxyContin, heroin or methamphetamine. People relapse. Overdose deaths haunt the nurses and counselors. They keep sticky notes on their computers to remind them of their successes: “I LOVE MY JOB — LOVE MYSELF.”
One patient who came in on a recent Wednesday said he knew of at least seven members of his high school football team — and 30 people at his school, including the homecoming king and queen — who died from overdoses.
Amid the wreckage, Julie Thompson, a nurse practitioner who grew up in the area, estimates that 75% of her addiction patients are currently housed, though not always consistently.
1

2
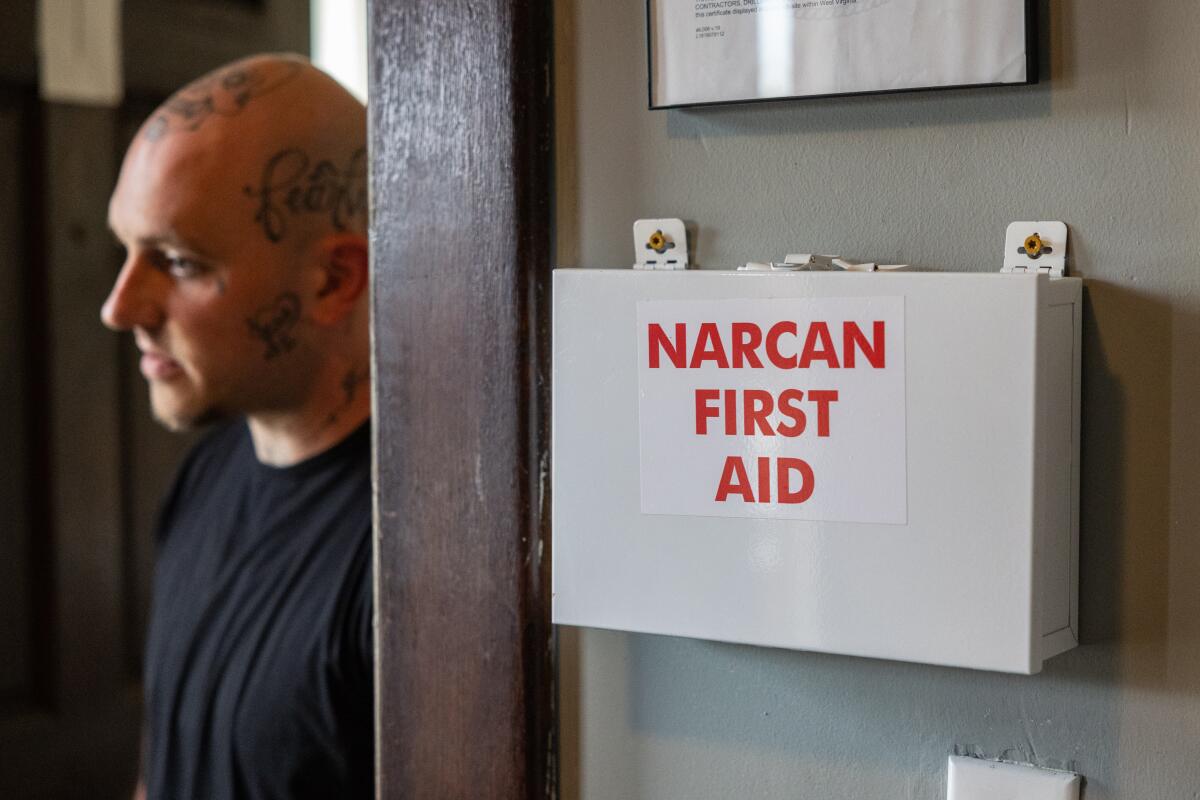
1. A patient of OVP clinic, which provides treatment for people with substance use disorders among other treatments. 2. Blake Orner stands in the doorway of his bedroom at Huntington Addiction Wellness Center. Orner has been in the program for four months after spending time battling addiction. (Jason Armond/Los Angeles Times)
“A lot just float from family member to family member to keep them off the street,” she said. “Some of [those relatives] are drug addicts themselves. So it’s kind of like — give me drugs and you can stay here.”
That codependence can prolong addiction.
But extremely low housing costs and long-term ties to the region make it possible for West Virginians to get by with less. The state has 50 affordable and available rental homes for every 100 extremely-low-income households, more than double the number that California has, according to a study by the National Low Income Housing Coalition.
An average family here can afford a modest two-bedroom rental on less than $17 an hour, the second-lowest figure in the nation. The same family would need to make more than $40 per hour to afford a two-bedroom rental in California, which has the highest costs, according to the coalition.

Candy Robinson, 42, said she never had a problem finding work or a place to stay during more than a decade of drug use, living mostly in a nearby coal-mining town where she grew up. Her family occupied a house in a coal camp where they had been living for generations, paying a nominal $16 a month in rent until she was in 11th grade, when it went up to $200. She stayed there and in trailers, sometimes with no electricity or running water, in the years she used drugs.
“I was a functioning addict. So I always had money and drugs,” said Robinson. “Everybody wanted to be my friend.”
Others struggling with addiction here have been able to maintain a higher standard of living. Thompson, the nurse practitioner, ticked off a list of people who had been in the clinic for treatment in recent days: a nurse, a surveyor, employees at the Toyota plant and a slew of truckers.

“It was just in my routine,” said Rodney Johnson, a 58-year-old cook who described his heroin habit while working in restaurants where he said drug use was rampant. “Get up, take a shot, go to work.”
Johnson said he “put his wife and family through hell,” sometimes disappearing for stretches when they had no idea if he was alive or dead. He lost his oldest son and oldest daughter to overdoses. He spent time behind bars, including four years on federal charges. But he never lost his home.

He often worked and his wife held a steady job with the state highway department, allowing them to pay about $900 a month in rent, even as they struggled to buy groceries. Last year, as Johnson began rebuilding his life, they bought a house for $65,000, with a $450-a-month mortgage.
It’s a two-story brick house, with a backyard and a grill on the porch along a cobblestone street. His neighbors across the street pay $400 a month in rent and fees to live in one of an estimated 70 sober houses sprinkled throughout the city.
The mix of cheap real estate and high addiction rates has led to a proliferation of these houses, which rent rooms to people fighting addiction who might otherwise struggle to pay a security deposit or pass a background check.

City officials, concerned that the houses were growing without proper regulations, approved an ordinance in September requiring the facilities to create exit plans so that patients aren’t dumped onto the street without recourse. Some of the operators had become almost predatory, profiting off tenants who sometimes are asked to surrender their benefits checks, said Sarah Walling, a City Council member and attorney with OVP.
“A roof over your head does not necessarily equal stable housing or a safe place to live, or a healthy place to live,” Walling said.

Walling pointed to Craig Hettlinger, a former Marshall University soccer player who started a recovery program after he stopped using drugs in 2018, as one of the good guys. Hettlinger, 41, runs an in-patient treatment program, operates recovery houses with counseling services and fixes up apartments for people who progress toward independent living.
His business depends on buying properties for as little as $4,000 to $6,000 — including former drug houses — and then fixing them up himself for another $20,000 or so.
Chuck Evans, who works for Hettlinger as a rehab counselor, lives in one of Hettlinger’s more expensive properties — a six-unit apartment building that went for $225,000.

Evans and his fiancee pay a combined $600 a month. Their clean two-bedroom unit has a full kitchen, a washer-dryer, a living room that holds Evans’ coin collection and a back room where he keeps several bicycles.
It’s a vast improvement for Evans, who spent six years homeless — living in camp sites, on couches and in “trap houses” with fellow drug users.
But Evans doesn’t want to stay at his current apartment much longer. He’s been looking for a fixer-upper that never had homeless people squatting in it because, he said, they are more likely to have stripped out the plumbing and electrical wiring.

On a recent Tuesday, he pulled up an auction website and pointed to a listing. He had put in a bid the night before to buy the house for $1,500.
Then he called his father, who offered to help pay for it, or whatever else he might find. “Get one dirt cheap,” his father instructed him.
More to Read
Sign up for This Evening's Big Stories
Catch up on the day with the 7 biggest L.A. Times stories in your inbox every weekday evening.
You may occasionally receive promotional content from the Los Angeles Times.








