Op-Ed: A COVID-19 vaccine is one thing. Getting Americans to take it is another
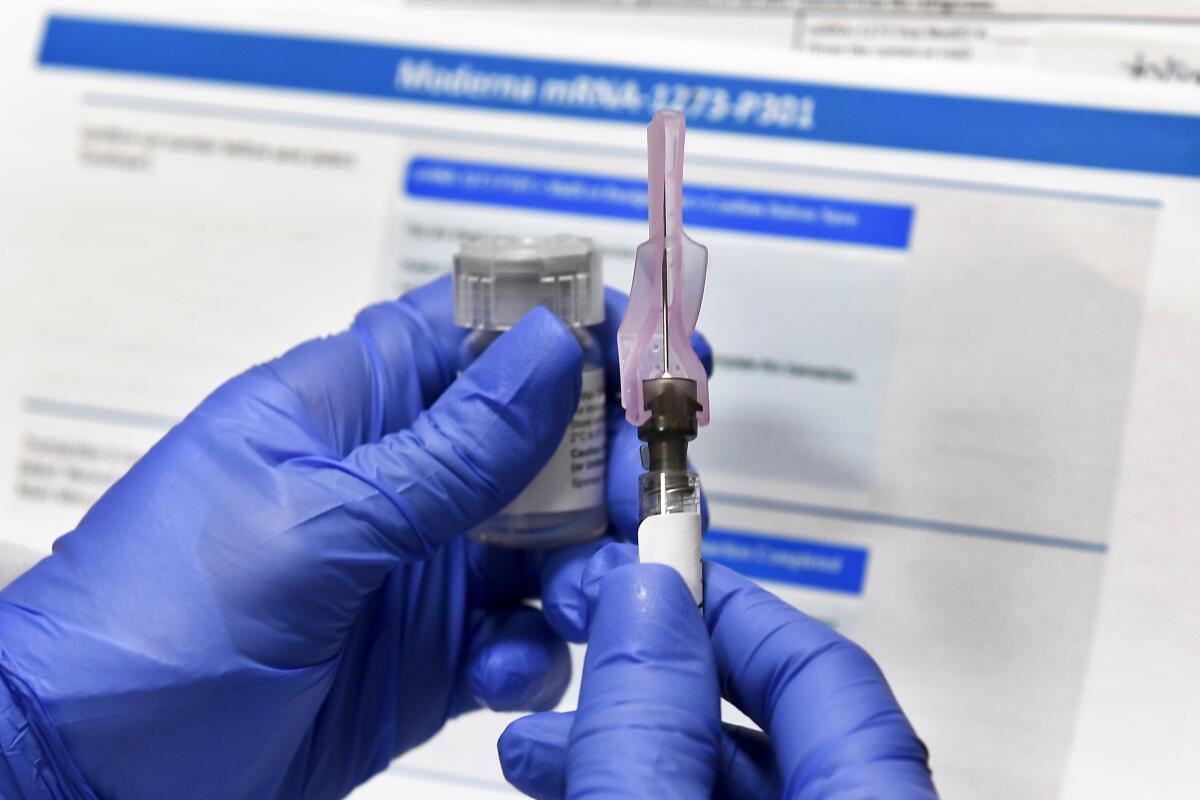
With multiple vaccine candidates in the late stages of clinical trials, it may seem that an end to the COVID-19 pandemic is just around the corner. But a safe and effective vaccine is merely the first step.
To attain herd immunity, a very large number of people must be vaccinated. This will require a prodigious global supply chain, equitable access to the vaccine and, perhaps most daunting in the case of the United States, the willingness of people to take it.
If getting Americans to wear a mask is hard, getting them to take a COVID-19 vaccine is likely to be even harder.
Despite overwhelming evidence that vaccines are safe, physicians routinely confront a resistance to vaccines of every stripe. According to the Centers for Disease Control and Prevention, only 62.6% of children under 18 and 45.3% of adults received the flu vaccine during the 2018-19 season. In 2018, only 51.1% of adolescents were up to date on their HPV vaccine, which prevents cervical and other types of cancer. Although it was declared eliminated in the U.S. in 2000, measles, a highly contagious disease that requires more than 90% vaccine coverage to achieve herd immunity, has made a comeback in the last decade.
We recently asked a demographically representative sample of 1,000 people from across the U.S. about their attitudes toward COVID-19, including their perceptions of vaccines. To our dismay, anti-vaccine sentiment was even more prevalent than expected.
There is a growing number of “vaccine hesitant” Americans who have not previously identified with the anti-vaxxer movement. Polls show that as the coronavirus pandemic has continued, citizens have become less confident about the safety of a vaccine.
Among survey participants, 36% said they thought vaccines have harmful effects that are not being disclosed to the public, 10.3% said childhood vaccines are not very safe or not safe at all, and 21.1% reported refusing vaccines in the past.
There was a bright spot: When it comes to a potential coronavirus vaccine, most respondents said they would look to medical experts for guidance. Asked to rate whose endorsement would affect their choice, 41.5% ranked public health leaders such as Dr. Anthony Fauci or Dr. Deborah Birx first, while 24% ranked their personal doctor first.
But an alarming portion of respondents — 21.8% — said they definitely would not get a coronavirus vaccination. Those with a lower level of education and those who identified as conservative were more likely to say they would refuse the coronavirus vaccine and would be less likely to listen to public health experts. Lower education level was also associated with higher likelihood of voting for President Trump in the November election.
Depending on the infectious disease, usually 70% to 90% of a given population must be immune to achieve herd protection. The vaccination rate required to achieve herd immunity depends on the effectiveness of the vaccine itself. The seasonal flu vaccine is only 60% effective at best. If the coronavirus vaccine is anything like the flu vaccine, a vaccination compliance rate of 100% would not be enough to reach herd immunity.
Our survey suggests that fewer than 80% of Americans may get vaccinated for the coronavirus. In this scenario, even if a new vaccine were 80% effective, which is optimistic, only 64% of the public would be protected. That doesn’t get us to herd immunity.
The situation is not hopeless. A protection rate of 60% would dramatically slow the pandemic in the U.S. But the reality is we depend on one another to reach vaccination levels that reduce risk. Not only do we need a safe and effective vaccine, then we need widespread acceptance of it.
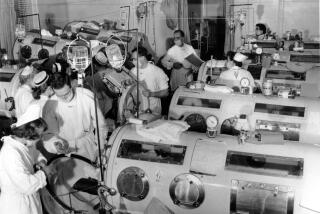
Successful vaccination campaigns in the past have relied on political endorsements and strong public-private partnerships. President Franklin D. Roosevelt played a crucial role in raising money for polio research well before the National Institutes of Health had a big budget.
President Eisenhower later used advice from the best scientists and physicians to assure the public that polio vaccines were safe and effective. Today, global polio eradication campaigns are led by national governments, global health agencies and private entities, such as the Bill & Melinda Gates Foundation. A disease that once devastated millions around the world is now endemic in only two countries.
Any future coronavirus vaccination campaign will require strong leaders who support good science, not leaders who manipulate or obstruct science for their own political agendas. The U.S. also needs to continue, not terminate, its working relationship with the World Health Organization and other global entities. This pandemic will not be over, in the U.S. or anywhere else, until an effective vaccine reaches every vulnerable community around the world.
Jiayin Xue is an adjunct professor at the Stanford Clinical Excellence Research Center and a pediatrician. Robert M. Kaplan is a distinguished research professor of public health at UCLA and adjunct professor at the Stanford Clinical Excellence Research Center. Previously he was an associate director of the National Institutes of Health and a chief science officer at the U.S. Agency for Healthcare Research and Quality.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.