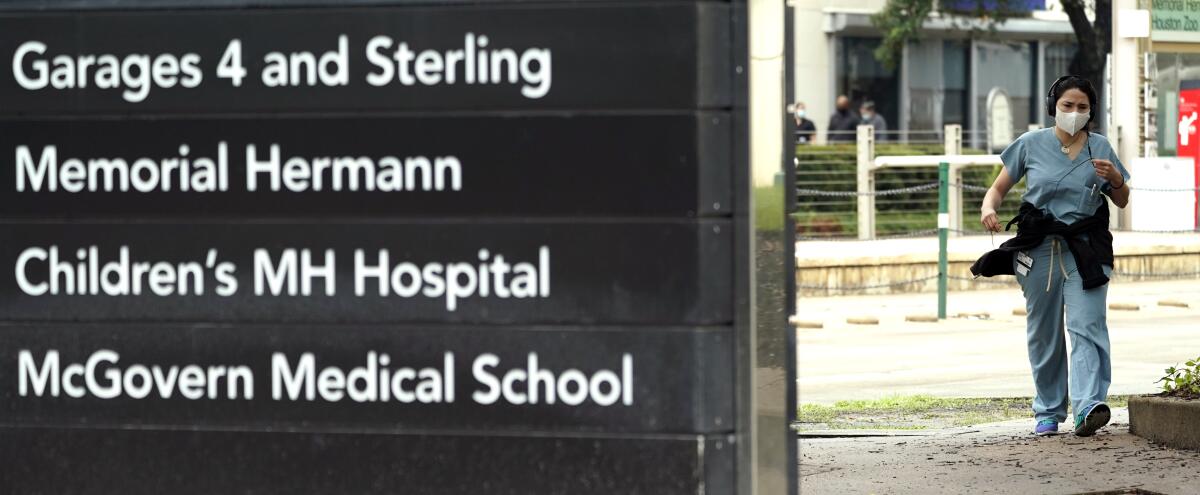
Wave of coronavirus threatens to swamp hospitals in Texas, Florida and other states
WASHINGTON — Just weeks after the coronavirus overwhelmed hospitals in and around New York City, medical centers in Arizona, Florida, Texas and other states with skyrocketing infections are rapidly filling with sick patients, threatening their healthcare systems.
The swift increase has forced hospital leaders to begin bringing in extra staff, converting space into dedicated coronavirus units and, in some cases, moving sick patients hundreds of miles to get to available beds.
Surging numbers of patients with COVID-19 — though still shy of the wave that hit New York — also raise the prospect of new restrictions on nonessential medical care to free up beds for patients infected with virus.
“The numbers are definitely scary,” said Judy Rich, chief executive of Tucson Medical Center, a hospital with more than 500 beds that serves patients from across southern Arizona. Tucson Medical Center has seen a threefold increase in COVID-19 patients since the beginning of June.
“When we started opening up the state, we immediately saw pictures of people packing into bars at night and celebrating,” Rich said. “It feels like we did too much too fast, and now we are paying the price.”
California, where infections are also soaring, is beginning to experience its own crush, with the number of hospitalized COVID-19 patients surging 32% in the last two weeks, Gov. Gavin Newsom reported Thursday.
The governors of Texas and Florida backpedal on their states’ aggressive reopenings amid resurgences of COVID-19 cases.
On Friday, the Trump administration tried to tamp down anxiety about the skyrocketing number of cases with the White House coronavirus task force holding its first public briefing in two months.
Vice President Mike Pence, who heads the panel, hailed increases in testing, broader distribution of medical supplies and a declining number of deaths. “We have made truly remarkable progress,” Pence said.
But Dr. Anthony Fauci, who heads the National Institute of Allergy and Infectious Diseases and who, unlike Pence, wore a face mask to the briefing, issued a more sober warning that Americans, particularly younger people, would need to take greater precautions to slow the spread of the virus.
“We are facing a serious problem in certain areas,” he said.
Across the country, hospital leaders, physicians and public health officials are issuing pleas for people to wear masks and keep distant from one another to slow the pandemic and prevent healthcare systems from collapsing.
In Arizona, as of Wednesday, 88% of the intensive care unit beds statewide were occupied, up from 68% in mid-May, according to state figures.
Banner Health, the state’s largest hospital system, is already deploying its surge plan, including hiring 200 new contract nurses to handle the increased demand.
In Texas, state health officials recorded 4,739 hospitalized patients with COVID-19, more than double the number just 10 days ago.
The steep rise prompted Gov. Greg Abbott, a Republican who has resisted placing restrictions on the state’s residents, to issue an executive order Thursday suspending elective surgeries at hospitals in the state’s largest counties, including those home to Houston, Dallas and San Antonio.
Abbott said the order was necessary “to help ensure that the hospitals in these counties continue to have ample supply of available beds to treat COVID-19 patients.” Abbott took another step Friday, ordering bars in the state to close except for food takeout service.
Florida, another emerging hot spot, is not reporting the number of hospitalized COVID-19 patients. (Republican Gov. Ron DeSantis, an ally of President Trump, for months has tried to downplay the severity of the pandemic.)
But Miami-Dade County — the state’s largest, which is reporting hospitalization data — recorded a new high Thursday, with 885 infected patients in hospitals, up from 546 two weeks ago.
“The trend is not reassuring,” said Kathleen Sposato, who oversees infection control at Jackson Health, the county’s mammoth safety-net medical system. “We are very, very concerned.”
The number of COVID-19 patients at Jackson Health has more than doubled since June 8.
The growing pressure on medical systems is not being felt everywhere.
In Jacksonville, Fla., Baptist Health, one of the largest medical systems in northern Florida, currently has only 24 COVID-19 patients, officials reported.
And Christus Health, a large system of Catholic medical centers across the South that includes 30 hospitals in Texas, isn’t nearing capacity, said Dr. Sam Bagchi, the system’s chief medical officer.
Bagchi compared the current demand at Christus hospitals to a busy flu season. “There are yellow flags, but the red ones aren’t there,” he said.
Even at more stressed systems like Tucson Medical Center, hospital officials noted that they are seeing younger, healthier patients with COVID-19 now, compared with earlier this year, which has made caring for them easier.
Advances in treatments, including the use of drugs such as remdesivir and dexamethasone, have also eased some of the burdens that hospitals experienced when the crisis first struck this year.
But health officials cautioned that the rapid spread of infection in places including Texas, Florida, Arizona and California means that even systems that have so far been spared are probably not safe.
“We can see the storm coming,” said John Henderson, who heads the Texas Organization of Rural and Community Hospitals.
Henderson noted that several member hospitals in suburban and rural areas around Houston are already being called on to take very ill patients from overburdened medical centers in the city, which is experiencing among the worst coronavirus outbreaks.
In California, hospitals as far north as Sacramento are taking COVID-19 patients from hospitals in Imperial and San Diego counties, which have been overwhelmed with expatriates coming home from Mexico for treatment.
Carmela Coyle, chief executive of the California Hospital Assn., said officials expect more patient transfers will become necessary as demand increases across the state. “Our sense is that we are a week to 10 days out,” she said.
Coyle said the hospital group is working with state officials on a surge plan to meet the anticipated increase in COVID-19 patients. One goal is to prevent the need for the kind of shutdowns that this spring sharply limited medical services for patients who were not infected.
But she and others also stressed that public engagement in preventing further spread of the virus will be critical to preserving access to hospitals.
“This is a community problem,” said Sposato, the Miami hospital official. “There needs to be a lot more community participation in this effort.”
More to Read
Get the L.A. Times Politics newsletter
Deeply reported insights into legislation, politics and policy from Sacramento, Washington and beyond. In your inbox three times per week.
You may occasionally receive promotional content from the Los Angeles Times.













