You are so done with this coronavirus lockdown.
You’re tired of Zoom cocktail hours, the never-ending pile of dishes, Netflix.
You miss your friends. You want to hug your parents. You want to see people’s faces, no masks please.
1/82
Socially distanced bikers and walkers, against a backdrop of the Queen Mary, make their way along pedestrian and beach bike path on the first day that Long Beach reopened the path on Monday May 11, 2020. The city of Long Beach eased a few of its public health restrictions, allowing under certain guidelines the reopening of pedestrian and beach bike paths, tennis centers and courts. Beach bathrooms are also reopening, but the parking lots and beaches still remain closed. (Genaro Molina/Los Angeles Times)
2/82
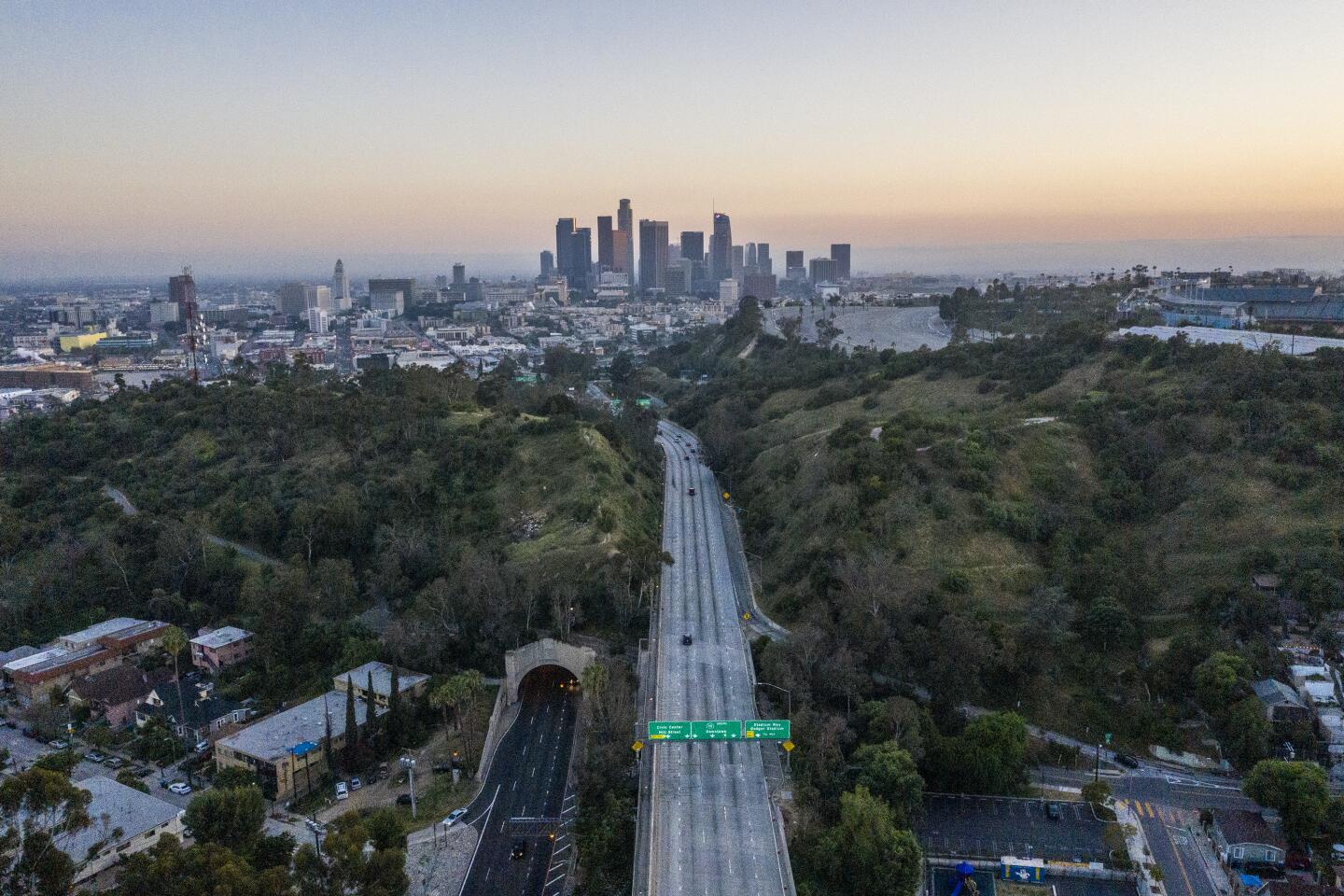
Traffic remains light on the southbound 110 Freeway headed toward downtown Los Angeles on April 28. (Robert Gauthier / Los Angeles Times)
3/82
Dominique Barrett, center, known as “King Vader” to his 2.4 million TikTok followers, prepares to shoot a video on April 30 in Glendora. (Dania Maxwell / Los Angeles Times)
4/82
Cody Purcell of Redondo Beach rides a wave, glowing from the bioluminescence, in Hermosa Beach, CA, after midnight Friday morning, May 8. (Jay L. Clendenin/Los Angeles Times)
5/82
Friends play spikeball, a game perfect for social distancing on an open but restricted San Buenaventura State Beach. (Brian van der Brug / Los Angeles Times)
6/82
The majority of golfers are wearing masks while hitting balls on the driving range at Van Buren Executive Golf Course in Riverside. (Gina Ferazzi / Los Angeles Times)
7/82
Beaches including Harbor Cove Beach were open but beachgoers were not supposed to be sitting on the sand. (Brian van der Brug / Los Angeles Times)
8/82
Tango instructor Yelizaveta Nersesova leads a Zoom tango event from her Los Angeles home April 27 that brought together hundreds of dancers from around the world. (Jason Armond / Los Angeles Times)
9/82
Grocery store workers, joined by United Food and Commercial Workers International Union Local 770 representatives and community members, hold a rally in support of strict social distancing on May 1 at a Ralphs store in Hollywood where 19 employees have tested positive for COVID-19. (Kent Nishimura / Los Angeles Times)
10/82
Mostly masked commuters keep their distance from one another on a Metro bus in downtown Los Angeles on April 29. (Gabriella Angotti-Jones / Los Angeles Times)
11/82
Gregory Kuhl, 69, heads home after a shopping trip in Hollywood on April 28. Big cracks in the street, cars parked in driveways blocking sidewalks and uneven pavement levels make navigating his route difficult. (Dania Maxwell / Los Angeles Times)
12/82
Tenants and their supporters from across Los Angeles gather at city hall to call on L.A. Mayor Eric Garcetti, the L.A. City Council and California Gov. Gavin Newsom to cancel rent and mortgage payments during the COVID-19 crisis. (Luis Sinco / Los Angeles Times)
13/82
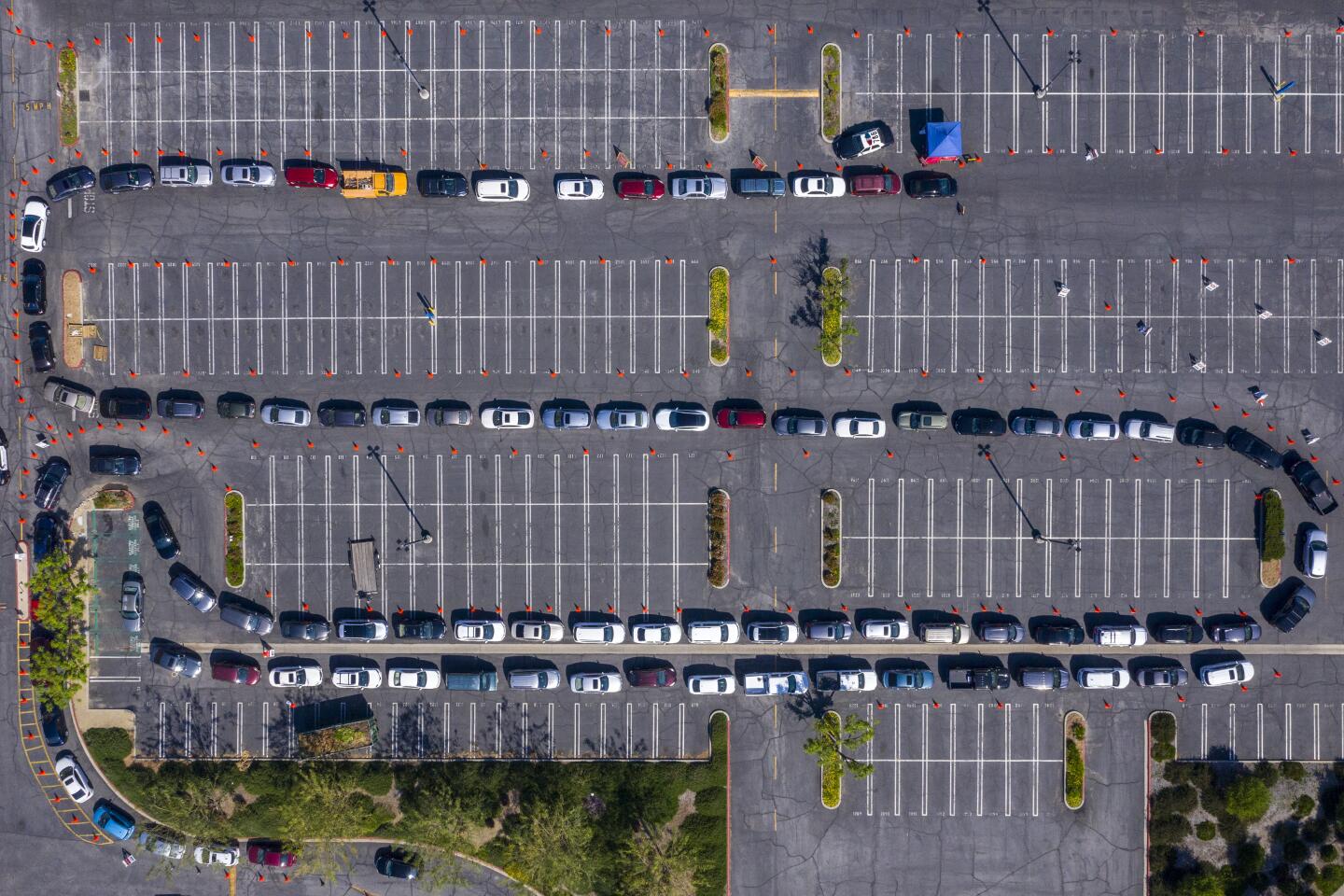
Aerial view of over 100 vehicles lined up at the West Valley COVID-19 testing center at Warner Center in Woodland Hills. (Brian van der Brug / Los Angeles Times)
14/82
Senior Mason Wise, left, helps his sister, Mackenzie, a sophomore, clean out her PE locker at El Camino Real Charter High School in Woodland Hills. School officials were allowing no more than five students at a time on campus to take home their belongings. (Brian van der Brug / Los Angeles Times)
15/82
Shuttered storefront businesses in the garment district of Los Angeles. California’s unemployment rate has skyrocketed since the statewide coronavirus shutdown took effect. (Luis Sinco / Los Angeles Times)
16/82
Healthcare workers celebrate as Claudia Martinez is discharged from the ICU after she recovered from COVID-19 at Scripps Mercy Hospital in Chula Vista. (Marcus Yam / Los Angeles Times)
17/82
Carson residents Kaeli Burks, 3, left, and her cousin Bailey Watson, 5, look out the window of their car after their mothers helped them with self-testing at a new drive-up testing site for COVID-19 in Carson. Free COVID-19 testing is available to all city residents thanks to a partnership between the city and US Health Fairs. (Genaro Molina / Los Angeles Times)
18/82
Norm and Tracy Kahn enjoy eating dinner outside on a small cafe table sitting in blue chairs on their side yard during the coronavirus pandemic on April 27 in Riverside. “During this pandemic, eating outside offers us an opportunity to change surrounding and appreciate the calmness of being outdoors among trees, scents from nature and the sounds of birds,” she said. Also adding, “Mixing up where we eat puts variety into our days and takes away the sameness of feeling trapped at home.” (Gina Ferazzi / Los Angeles Times)
19/82
Ronald Reagan UCLA Medical Center nurses carry supplies outside the hospital. (Robert Gauthier / Los Angeles Times)
20/82
Tom Sean Foley pauses on a walk with his kids, Cathelen Claire, “C.C.,” 3, and Timothy Joseph, 4, to take a photo in front of the “Love Wall,” mural by artist Curtis Kulig, outside of Smashbox Studios in Culver City. (Jay L. Clendenin / Los Angeles Times)
21/82
Protesters stand along Mission Blvd. in Pacific Beach during A Day of Liberty rally on April 26. The protesters were against the government shutdown due to the coronavirus. (K.C. Alfred / San Diego Union-Tribune)
22/82
People make orders at a food truck along Shoreline Avenue in Long Beach. (Luis Sinco / Los Angeles Times)
23/82
Medical staff, wearing protective gear, work inside a COVID-19 isolation area inside the emergency department at Los Angeles County-USC Medical Center in Los Angeles, where patients with the virus are being treated. (Mel Melcon / Los Angeles Times)
24/82
Neighbors practice social distancing while enjoying the nice weather near The Strand in Hermosa Beach. (Gabriella Angotti-Jones / Los Angeles Times)
25/82
Counter-protesters attend a protest to call on state and local officials to reopen the economy in downtown Los Angeles. (Christina House / Los Angeles Times)
26/82
A group of protesters cheer on cars during a vehicle caravan protest to call on state and local officials to reopen the economy in downtown Los Angeles. (Christina House / Los Angeles Times)
27/82
Cedar Mountain Post Acute Rehabilitation staff member Navi Cavaltera waters a flower pot put up by the community to show their support for the nursing staff of the facility in Yucaipa. Eighteen of 20 coronavirus-related deaths in Yucaipa were residents of the skilled nursing facility. (Irfan Khan / Los Angeles Times)
28/82
A pedestrian wearing a protective mask passes a mural on a store on Melrose Avenue in the Fairfax district of Los Angeles. (Allen J. Schaben / Los Angeles Times)
29/82
Jonte Florence, a freestyle dancer, does a handstand on a mostly empty Hollywood Walk of Fame. Florence said he normally performs for hundreds of tourists along the busy street. (Allen J. Schaben / Los Angeles Times)
30/82
The Tyrannosaurus rex overlooking the intersection of Hollywood Boulevard and Highland Avenue wears a protective mask while practicing social distancing. (Allen J. Schaben / Los Angeles Times)
31/82
Businesses are shuttered and pedestrians are few and far between on Hollywood Boulevard. (Allen J. Schaben / Los Angeles Times)
32/82
Daniel Rogerson wears a vintage military gas mask while riding a bike along the beach path in Santa Monica, which is closed to enforce social distancing because of the coronavirus pandemic. (Luis Sinco / Los Angeles Times)
33/82
A face mask seller in colorful dress appears to be part of a mural behind a bus stop on Soto Street in Los Angeles. (Irfan Khan / Los Angeles Times)
34/82
Life around Cesar E. Chavez Boulevard and Soto Street has slowed down as California officials extended stay-at-home orders into May and residents entered Easter weekend with unprecedented limits on their movements. (Irfan Khan / Los Angeles Times)
35/82
UC Irvine Medical Center health care workers return their gratitude as about 25 Orange County first responder vehicles participate in a drive-by parade of gratitude as they battle COVID-19 at the hospital. (Allen J. Schaben / Los Angeles Times)
36/82
Billy Budd, 55, of Hollywood, walks along Hollywood Boulevard with a protective face covering. Budd is a scenic artist for movies and television who is currently out of work due to the coronavirus outbreak. (Mel Melcon / Los Angeles Times)
37/82
Stuart Reyes and his sister, Stephanie, sell masks for $5 each on the 3000 block of West Century Boulevard in Inglewood. Stuart Reyes said he is selling masks to support his mother. (Irfan Khan / Los Angeles Times)
38/82
A jogger runs on a closed trail past dozens of pieces of caution tape, torn off by hikers and mountain bikers at El Escorpion Canyon Park in West Hills. (Brian van der Brug / Los Angeles Times)
39/82
Alex Herron and nurse Mercy Pineda at a blood drive sponsored by USC athletics and the American Red Cross at USC’s Galen Center. (Genaro Molina / Los Angeles Times)
40/82
Los Angeles City Hall displays blue lights to show support for healthcare workers and first responders. (Gary Coronado / Los Angeles Times)
41/82
After being indoors for several days because of rainy weather and coronavirus stay-at-home orders, Olivia Jacobs, 4, and her mom, Cia Jacobs, enjoy a warm and sunny afternoon making chalk drawings on the sidewalk in front of their home in West Hills. (Brian van der Brug / Los Angeles Times)
42/82
An Oceanview Plaza security guard sports a whimsical mask while on patrol. (Robert Gauthier / Los Angeles Times)
43/82
Jacob De Wilde, left, and Lesli Lytle load a car with food during a food distribution organized to mark Good Friday. (Irfan Khan / Los Angeles Times)
44/82
As a late season storm continues to make its way across the Southland, a young basketball player dribbles along an alley through an Elysian Park neighborhood in Los Angeles. (Kent Nishimura / Los Angeles Times)
45/82
People are silhouetted in a window of an apartment building in Hollywood, where a stay-at-home order remains in effect to help curb the spread of the coronavirus. (Luis Sinco / Los Angeles Times)
46/82
The Wilshire Grand Center display blue lights and a heart to show support for healthcare workers and first responders. (Gary Coronado / Los Angeles Times)
47/82
Women wear masks as they stroll along Highland Avenue in Hollywood. Wearing masks while outdoors is mandatory in the city of Los Angeles. (Luis Sinco / Los Angeles Times)
48/82
Patients are removed from Magnolia Rehabilitation and Nursing Center after 39 tested positive for the coronavirus and nursing staff was not showing up to work. (Gina Ferazzi / Los Angeles Times)
49/82
A specimen is turned in at the new mobile testing site for people with symptoms of the coronavirus at Charles R. Drew University of Medicine and Science in South Los Angeles. (Christina House / Los Angeles Times)
50/82
Hippie Kitchen in Los Angeles hands out food, water and toiletries to homeless people and residents of skid row. Additionally, masks were offered to help reduce the spread of the coronavirus. (Myung J. Chun / Los Angeles Times)
51/82
Nurses pose for a fun photo during a break in drive-through public testing for the coronavirus at Arrowhead Regional Medical Center in Colton. (Irfan Khan / Los Angeles Times)
52/82
A woman shows a notice from her doctor that allows her to obtain a test for coronavirus at a new drive-up testing site in a parking lot at the South Bay Galleria in Redondo Beach. (Genaro Molina / Los Angeles Times)
53/82
A person who wishes to remain anonymous strikes from her car to support McDonald’s employees who are demanding the company cover healthcare costs of any worker or immediate family member who gets sick from COVID-19 in Los Angeles. (Dania Maxwell / Los Angeles Times)
54/82
Cassidy Roosen, with Beach Cities Health District, holds up a sign that says, “We’re All in This Together,” while waiting to direct cars at a drive-through, appointment-only coronavirus testing location at the South Bay Galleria in Redondo Beach. (Jay L. Clendenin / Los Angeles Times)
55/82
Grace Carter, 15, of Riverside, practices a dance routine at home after dance classes and school were canceled. She has to use the Zoom app on her iPhone to practice with her dance group. “It’s hard,” she said. “My bedroom is a smaller space. I miss all my friends at the studio.” (Gina Ferazzi / Los Angeles Times)
56/82
A man works from his home in Long Beach. (Marcus Yam / Los Angeles Times)
57/82
A San Bernardino County healthcare worker takes a sample at a coronavirus drive-through testing site at the county fairgrounds in Victorville. (Irfan Khan / Los Angeles Times)
58/82
A Metro general service employee disinfects a bench in Boyle Heights. (Gary Coronado / Los Angeles Times)
59/82
A runner jogs past the Pottery Barn in Pasadena. Some businesses in the area have boarded up their stores. (Al Seib / Los Angeles Times)
60/82
Raquel Lezama and daughter Monica Ramos collect meals for their family at Manual Arts High School. Lezama was laid off from her $17.76-an-hour job at a Beverly Hills hotel. (Al Seib / Los Angeles Times)
61/82
The Iron City Tavern in San Pedro tries an incentive to lure takeout customers. (Carolyn Cole / Los Angeles Times)
62/82
Healthcare workers gather outside UCLA Ronald Reagan Medical Center to call for further action from the federal government in response to the COVID-19 outbreak. (Robert Gauthier / Los Angeles Times)
63/82
Kristen Edgerle, of Victorville, collects information from a blood donor before drawing blood at The Richard Nixon Presidential Library blood drive during the coronavirus pandemic in Yorba Linda. (Jason Armond / Los Angeles Times)
64/82
Shauna Jin, of Los Angeles, with her dog, Bodhi, practices social distancing with John Kiss, of Los Angeles, at the entrance of Runyon Canyon Park in Los Angeles. (Gary Coronado / Los Angeles Times)
65/82
A lending library had some additional useful items, including a roll of toilet paper and cans of beans and corn, in a Hermosa Beach neighborhood. (Jay L. Clendenin / Los Angeles Times)
66/82
Protesters drive by the Getty House, the home of L.A. Mayor Eric Garcetti, in Hancock Park. Tenant advocates are demanding a total moratorium on evictions during the coronavirus crisis. (Wally Skalij / Los Angeles Times)
67/82
Venice residents Emily Berry and Gavin Kelley take a break at Venice Beach. Berry, a cocktail waitress at Enterprise Fish Co., lost her job due to the coronavirus outbreak. Kelley, a manager at a performing arts school with a focus on music, said that he still has a job and that classes at the school will resume online this coming Monday. (Mel Melcon / Los Angeles Times)
68/82
The JW Marriott at L.A. Live is sharing a message of hope with red lights in 34 windows, creating a 19-story display on the hotel’s north side. (Gary Coronado / Los Angeles Times)
69/82
Juan Diaz Jr., a lifelong Dodgers fan, prays that the season will start by May in front of Dodger Stadium on what would have been opening day. (Mel Melcon / Los Angeles Times)
70/82
Hayley, CEO and founder of Love My Neighbor Foundation, right, dances with Crystal Armster, 51, while she and her colleagues continue to feed the homeless on skid row amid the pandemic. (Genaro Molina / Los Angeles Times)
71/82
A masked passenger on a Metro bus in downtown Los Angeles. (Wally Skalij / Los Angeles Times)
72/82
Dede Oneal waits for a coronavirus test at the Crenshaw Christian Center in South Los Angeles. (Genaro Molina / Los Angeles Times)
73/82
A man in a mask passes a closed restaurant along Spring Street in downtown Los Angeles. (Wally Skalij / Los Angeles Times)
74/82
Artist Corie Mattie paints a mural on the side of a pop-up store as a man takes a picture in West Hollywood. (Wally Skalij / Los Angeles Times)
75/82
Medical assistant Zoila Villalta works with Rosie Boston, 32, of Glendale, who is donating blood for her first time at L.A. Care Health Plan downtown. (Al Seib / Los Angeles Times)
76/82
A couple wait for a bus outside the Petersen Automotive Museum in Los Angeles. (Luis Sinco / Los Angeles Times)
77/82
With all Los Angeles schools closed until further notice, LAUSD buses sit idle in Gardena. (Brian van der Brug / Los Angeles Times)
78/82
A lone traveler makes his way to catch a flight in Tom Bradley International Terminal. (Genaro Molina / Los Angeles Times)
79/82
Denise Young looks on as her daughter, Allison, 9, a fourth-grader at EARThS (Environmental Academy of Research Technology and Earth Sciences) Magnet School in Newbury Park, receives a Chromebook. (Mel Melcon / Los Angeles Times)
80/82
Hollywood Boulevard is devoid of the usual crowds. (Brian van der Brug / Los Angeles Times)
81/82
Michael Ray, 11, plays before a movie at the Paramount Drive-In. (Wally Skalij / Los Angeles Times)
82/82
Isabella Leader, 15, counts how many flags have been left for World War II veteran Lt. Col. Sam Sachs who was celebrating his 105th birthday at the Mom & Dad’s House, an assisted living facility, in Lakewood. Lt. Col. Sachs appealed to the public for birthday cards after the coronavirus pandemic forced the cancellation of a big celebration and wound up receiving thousands, including a letter and photo from President Trump. (Genaro Molina / Los Angeles Times)
And if you are among the more than 30 million Americans who filed for unemployment since mid-March, you are probably freaking out about your finances too.
Perhaps you are beginning to wonder if the people protesting stay-at-home orders around the state and across the country have a point: Maybe this extended physical distancing is doing more harm to our collective health than good.
Just how bad would it be to let everyone struggling to pay their bills go back to work? To eat at a restaurant again? To go to the beach on a hot day without being scolded by your governor?
After all, doesn’t this pandemic end with either a vaccine, herd immunity or some combination of the two? If everything reopened and a few more people got sick, might that be a reasonable price to pay?
If only it were that simple.
There is no doubt that there are significant health risks associated with the lockdown. People fearful of going to the hospital or the doctor’s office are delaying cancer treatments, toughing out strokes and heart attacks at home and thinking about skipping their dialysis sessions.
Studies show that in times of economic hardship suicide rates go up and domestic violence increases. And prolonged physical isolation is associated with an increase in depression, anxiety, irritability and stress.
But for the time being, public health experts say those costs cannot compare with the massive loss of life that would occur if officials decide to throw up their hands and fast-track herd immunity.
Nearly 60,000 Americans died of COVID-19 in April, and that was when physical distancing measures were largely in place across the country.
By comparison, researchers estimate that the Great Recession that began in December 2007 led to 4,740 additional suicides in the U.S. over the ensuing three years.
Even if you include deaths from other causes that might be tied to a bad economy, “I don’t think there is a great data-driven argument that any recession is likely to cause the same amount of death as we are currently seeing from COVID-19,” said Dr. David Eisenman, director of UCLA’s Center for Public Health and Disasters. “That would have to be examined, but that’s my hypothesis.”
And scientists say that if lockdown restrictions were suddenly lifted, the number of deaths from the virus would skyrocket.
“As a country, we are certainly talking about at least a million deaths if we just reopen and do nothing else,” said Ira Longini, a professor of biostatistics at the University of Florida.
“You can try to do a cost-benefit analysis, but it’s hard to put a dollar value on death,” he said.
Longini’s models suggest that by the end of April, between 3.4% and 6.3% of the U.S. population had been infected with the virus.
Achieving herd immunity would require at least half of the population to have immunity to the virus, and ideally more like 60% to 70%, he said.
And it’s not clear that surviving an infection will do much to build herd immunity. Scientists don’t know yet how long immunity to COVID-19 lasts: It could be years, or it could be months. It’s also possible that it might not exist at all.
If the virus acts like other coronaviruses, it’s probable that people will have at least partial immunity for several months after recovering from an infection, but nobody can say that for sure, researchers said.
“The entire concept of herd immunity assumes something about COVID-19 we don’t know is true,” said Summer Johnson McGee, dean of the University of New Haven’s School of Health Sciences. “It’s a dangerous policy to float when we don’t have the immunological information that we need.”
Epidemiologists also caution that the blind pursuit of herd immunity would probably have the gravest consequences for the most vulnerable members of our society.
“We have huge inequities between rich and poor, black and white, and entire swaths of the country without insurance and access to doctors,” Eisenman said. “If we allow this disease to run through the population, it will no doubt take the poor and the most marginalized people in the society.”
It’s for these very reasons that epidemiologists say the United States should not pursue the strategy being carried out in Sweden. The northern European country has chosen not to close schools, restaurants and bars, and is instead relying on “trust-based” measures to control the virus. That includes advising people to work from home if they can, wash their hands regularly and avoid nonessential travel. Compliance, however, is voluntary.
It may sound like a dream, but health experts point out that the U.S. and Sweden are very different countries. For example, Sweden provides universal healthcare to its citizens as well as subsidized housing and child care.
“We’re not Sweden,” Eisenman said. “They did that in a society that has all these supports for people, and on top of that has excellent infrastructure for staying home.”
That being said, scientists are just as eager as the rest of us to get lockdown measures lifted as soon as possible, and most of them agree that keeping us stuck in our homes until a vaccine is found is not a viable strategy.
“This is something we’ve been discussing internally at the World Health Organization,” said Dr. Michael Ryan, executive director of the WHO’s health emergencies program. “On one hand we have the science, on the other hand we have the practical reality of life.”
Ryan said that until there is a vaccine, we may never reach a point when there is absolute scientific certainty that it is 100% safe for 20 people to be together in the same room — let alone 200 or 20,000.
Instead, he said government leaders and the communities they serve need to decide what risks they are willing to take and how they will manage the fallout if their risky decisions don’t pan out.
“This has to be considered on a societal level,” he said. “It has to be based on evidence, but you have to adapt that evidence to the reality of living life.”
Lydia Bourouiba, a professor of environmental engineering at MIT who studies the spread and control of infectious diseases, said the criteria for lifting lockdown measures should not be as strict as ensuring that nobody will be sickened by the coronavirus. Instead, the goal should be ensuring that the number of people who will need to be hospitalized with COVID-19 matches the capacity of local hospitals to care for them.
“The hospitals are really the bottleneck here,” she said.
Shelter-in-place orders have effectively kept many hospital systems across the country from becoming overburdened by COVID-19 patients, but that could change quickly as restrictions are eased.
“Because of confinement, there is an appearance that we can manage this,” Bourouiba said.
But if those measures were suddenly lifted with nothing to replace them, we would overwhelm the healthcare system and doctors would start having to choose who lives and who dies, she said.
“That’s the ethical question people in our society need to be thinking about,” Bourouiba added.
So, what will it take to ease the stay-at-home measures with minimal risk to society? Public health experts agree on the essentials: the capacity to rapidly test people who may be infected, isolate those who test positive, and track and quarantine their close contacts.
And unfortunately, communities must be willing to go back into lockdown if there is an explosion of cases in their midst.
“We are not going to get rid of this disease anytime soon, so we are going to have to learn to live with it,” Eisenman said.