CDC’s top COVID doctor explains how travelers can reduce risk in a mask-optional world

Your bags are packed, you’re ready to go. You’re standing there, outside your door. And you’re thinking, “If I catch COVID-19 on this trip, I could get seriously ill or die.”
You got a fresh N95 respirator for the trip. And you were counting on most of your fellow travelers to cover their noses and mouths too: the driver of your ride-share, the people in the airport, and passengers packed tightly inside the plane.
But this week, a federal judge in Tampa, Fla., issued an order that voided the Centers for Disease Control and Prevention’s mask mandate for those on public transportation. The U.S. Justice Department is appealing the decision at the CDC’s behest. Until the issue is sorted out in court, most commercial airlines, airports, buslines and public transit systems have stopped requiring travelers and employees to mask up.
That means you’re likely to be surrounded by maskless faces.
The ruling abruptly halted one of the pandemic’s most hotly contested public health measures. Its implications may be long-lasting.
The most transmissible strain of the coronavirus yet — the BA.2 subvariant of Omicron — dominates the landscape now. It may be slightly less lethal than its forerunners. But older people, those with medical conditions, and the unvaccinated face a heightened risk of serious disease or death if they become infected. While full vaccination offers some protection against becoming severely ill, that protection is leakier if you haven’t been boosted, or if your last shot was more than four months ago.
Now what do you do? Dr. John Brooks, the CDC’s chief medical officer for the COVID-19 response, has some practical advice:
Arm yourself. Get vaccinated, and if you’re fully vaccinated, get boosted. If you’ve had two or three shots of Pfizer’s Comirnaty or Moderna’s SpikeVax vaccine and it’s been four months since your last shot, another dose is advised. Give yourself a week or so for another jab to refresh your immune system’s supply of antibodies.
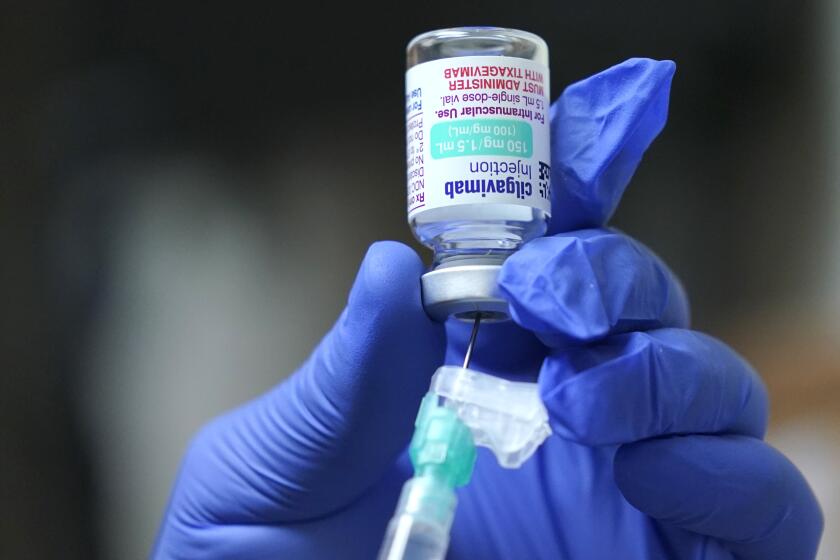
If you have certain medical conditions, can’t be vaccinated, or take medications that weaken your immune system’s ability to fight off infections, see if you can get a dose of Evusheld, a form of passive defense that can help protect you.
Patients in active treatment for cancer, or people who received a stem cell transplant for blood cancer in the past two years, may not have mounted a strong response to the vaccine. They need the extra boost of immunity that the monoclonal antibodies in Evusheld provide. Patients who take long courses of high-dose steroids or a range of other medications to treat auto-immune diseases such as lupus, rheumatoid arthritis or multiple sclerosis may be in the same boat. And anyone who has had a solid organ transplant needs more protection to compensate for the powerful medications they take to prevent rejection.
Evusheld can help protect immunocompromised people from COVID, but patients say scant awareness and a complicated process have hampered its rollout.
Just over a million doses of the protective medication have been distributed, mainly to hospitals and healthcare systems across the country. That won’t cover everyone who probably needs it. If you think it could help you, the rheumatologist, oncologist or transplant team that treated you is best positioned to help you get it.
Do wear your mask, and make sure it’s a good one. In a crowd, the more people are masking, the less virus will be suspended in the air to be breathed in, so more masking is better. But correct and consistent wearing of a mask that molds close to your face can protect you from breathing in those lingering viral particles, or limit how much you take in. That, in turn, could mean the difference between warding off infection and becoming ill.
You’ve heard this before, but it’s worth repeating: A cloth mask won’t cut it, given how readily the Omicron variant spreads. If you love your cloth mask, put a disposable surgical mask over it: they’re designed to draw in and trap virus on their surface. But your best bet is to wear an N95 respirator, which pinches around your nose and has ear loops or head straps that hold the mask tight to your face.
Many experts stress that face coverings still protect against the coronavirus and that masking up makes sense — even if it’s no longer mandatory.
“Before you go on an airplane, practice at home to make sure you can wear it comfortably, correctly and consistently,” Brooks said. “They’re itchy and scratchy and the air is hot for some people. But millions of healthcare providers have learned how to wear them, and you can too.”
Mind the transitions, and take a direct flight if you can. The filtration systems of most commercial jets are fully engaged when they’re traveling above 10,000 feet, Brooks said, and they are powerfully effective at cleaning the air under those conditions. But when jet engines are idling on the ground (and passengers are boarding or deplaning), those systems are not doing that job. And the efficiency of those air filtration systems also suffers as the plane ascends or descends.
So be sure to wear your mask during those transitions. And taking direct flights where possible limits the amount of time you’re sitting in a crowded metal tube with a filtration system that’s going to let more virus slip through than it will at cruising altitude.
Reserve a window seat, board last, and sit near the front so you can deplane quickly. The principle here is to spend the least amount of time possible on a plane that’s still on the ground, Brooks explained. You also want to sit where any virus emitted by passengers and staff in the aisles is least likely to reach you.
Seeking special favors from airlines is either costly or difficult. But most will let you choose your seat for an extra charge, and if you can do that, look for one that gives you some distance from passers-by but also lets you make a fast get-away.
Despite recent changes at the federal level, L.A. County continues to require travelers to mask up at airports and on public transit.
Eat or drink with caution. You’ll probably be hungry and thirsty if you’re taking a long trip. But if other travelers are largely unmasked, your snack or swig of soda is an opportunity for their virus to enter your respiratory tract.
Brooks notes that a straw can be inserted right under a mask, limiting the broken seal. He suggests eating in the airport rather than on the plane, and munching your meal in an unpopulated corner of the gate area. Wash your hands before eating.
Know the community transmission level where you’re going, and behave accordingly. Going to a hotspot of new cases, or passing through one on the way to your destination? Find out before you go so you know where masking and social distancing are still a good idea and where you can afford to loosen up. Visit the CDC’s community website and click on the counties you’ll be traveling from, to and through.
Stock up on rapid tests and prepare to spring into action if you have a positive result. It makes sense to test yourself before you travel, to make sure you’re good to go. But bring another test and take it four days or so after you’ve been in a high-exposure situation like an airport, or if you develop COVID-19 symptoms.
Getting the earliest possible indication of infection is all the more important because antiviral medications such as Paxlovid and molnupiravir are now available, and they can shorten the duration and/or lessen the severity of an infection. But they must be taken as soon as symptoms start, and no more than five days after symptom onset.