California once quelled COVID with stay-at-home order. Why this one isn’t working as well

California’s first coronavirus lockdown order, in the spring, produced benefits within a month. By April, Gov. Gavin Newsom was able to crow that the state had “arguably flattened” the curve on infections.
It has been two weeks since a second stay-at-home order was issued, and no such flattening has occurred across most of California. This may be because restrictions are looser than those in the spring, and because many Californians are so fatigued by public health orders — or militantly resistant to them — that they are mixing with people from outside their households.
But experts say the most pertinent explanation has to do with the amount of the coronavirus in the community. The latest order came after the virus was already raging out of control, in part because of Thanksgiving travel — a difference experts say will make the current surge much harder to corral.
ICU availability in Southern California at 0%, and the crisis is expected to get worse, officials warn.
“The virus is unforgiving and relentless, and there is just so much community transmission,” said Dr. Tomás Aragón, who next month will take over as director of the California Department of Public Health.
When new daily case counts reach more than 20 per 100,000 people, “it becomes really difficult to control the infections,” said Aragón, who has helped lead San Francisco’s pandemic response as the county’s health officer.
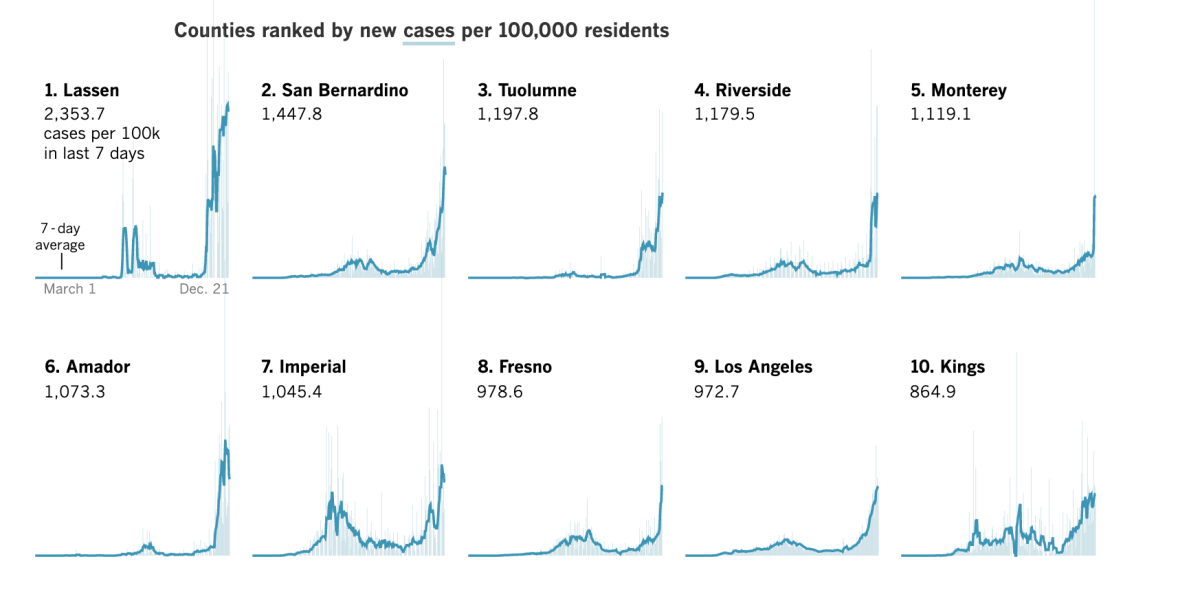
California’s daily case rates are soaring way beyond that number. Los Angeles County’s daily case rate last week was 153.6 per 100,000 residents, Aragón said. The state’s count was 82.2 per 100,000 residents, compared with a national average of 64.6.
“Once the rates get really high,” said Aragón, “it is not like you can fine-tune it with levers.”
The new stay-at-home order is making some difference, though. GPS data from cellphones show that people in California are moving around less, Newsom has said. Greater rates of movement have been associated with higher case counts throughout the pandemic.
Health experts interviewed by The Times said the situation would be even more dire without the new stay-at-home order. But their predictions of when cases might stabilize or dip — if only briefly — varied, ranging from a week to after the holidays.
Meanwhile, intensive care units at many hospitals are filled, and medical providers are being more selective about which patients are admitted.
Grocery stores and other essential businesses have been hit hard by the coronavirus surge, further straining services that must stay open despite the stay-at-home order.
The crush is expected to get worse before it gets better. Experts say the lack of hospital space and shortage of staff will lead to more deaths, not just for COVID-19 patients but also for people with other ailments who should have been hospitalized but were not able to gain admittance. The state has ordered thousands of body bags and refrigerated storage units to handle the dead.
Contrast this misery with the state’s success in the spring, when California reaped nationwide praise for flattening the curve by shutting down in March, closing all schools and nonessential retail. But the number of infections then, while rising, was only a fraction of what the state faces today.
“There is no precedent for how well a lockdown will work when you are having as many cases as we are currently having,” said Dr. John Swartzberg, an infectious-disease expert at UC Berkeley.
This new phase in the pandemic means new rules for hotels and other travel providers.
Dr. Robert Kim-Farley, a UCLA medical epidemiologist, likened the spread of the virus early in the pandemic to “lighted matches being thrown into the forest, which occasionally resulted in flare-ups.”
The March shutdown flattened the curve in three weeks, he said. Now, there is a “full-blown, raging, viral wildfire,” and “it’s just going to take longer” to bring it under control.
The match that ignited the fire was Thanksgiving. Many who traveled or gathered with people from outside their households got sick, then infected others. Additionally, cooler weather has made the environment more hospitable for the coronavirus, which thrives in low humidity and spreads more easily indoors.
Several experts said the surge from Thanksgiving may ebb by Christmas, with a flattening or even a dip in new cases. But gatherings for Christmas and New Year’s Eve may bring another wave of infections.
“I don’t think we will see a substantial drop in cases until sometime in the third week of January,” Swartzberg said.
For health orders to work, people must follow them, and compliance in some places has been spotty.
Inside the Promenade Temecula mall last week, business appeared brisk. Shopper Josie Cardenas, 23, a resident of Perris, said she had not expected the mall to be so busy and wished people would take the health orders more seriously.
“This is nothing like the past orders,” said the laid-off health worker. “Everything is open still, and people are going out.”
Fatima Tomlinson, 21, who went to the mall to buy hoodies that were unavailable online, said the stay-at-home order should be stricter.
“People are partying around us, they aren’t really abiding by the rules, and now they have an excuse to go out in public for the holidays,” said the Perris resident.
Riverside County Sheriff Chad Bianco has called the stay-at-home order “flat-out ridiculous.” He said in a video this month that his department would not enforce it.
Riverside County, which includes Temecula and Perris, had some of the highest per capita case and death rates of California’s 58 counties in the last week — even worse than hard-hit L.A. County.
In Northern California, at the Broadway Plaza in Walnut Creek, a popular open-air shopping destination usually jammed before Christmas, masked shoppers strolled the streets in vastly fewer numbers than in past years.
Lines of about half a dozen masked people formed outside Lululemon. Santa Claus waved from an outdoor perch. A masked elf said Santa had a mask under his white whiskers, but children could forgo face coverings while being photographed.
In Los Angeles County, unions for teachers, nurses and grocery and hotel workers have called for stricter health orders, including a shutdown in January. They implored the Los Angeles County Board of Supervisors for tougher action and started an online petition drive.
“Let’s be clear,” said United Teachers Los Angeles President Cecily Myart-Cruz. “We are not in a real lockdown.”
Reflecting the desperation of teachers, healthcare workers and hotel employees, their influential unions call for a strict month-long county shutdown to control COVID-19. New surveys describe the despair of teachers and parents.
Despite the frustration, none of the health experts interviewed by The Times said the state should have imposed a stay-at-home order as strict as the one in the spring, when nonessential retailers were barred from even curbside sales.
This time, Swartzberg said, “I think we have done it more intelligently.”
UCLA’s Kim-Farley noted that people flocked to big-box stores during the spring shutdown because they carried groceries and could stay open. Now, shoppers are spread out more evenly among many stores, which are limited in the number of customers they can allow inside.
Aragón said there is no easy answer.
“You need to have some economic activity for society to have social health,” he said. He believes many transmissions are coming from within households. An infected person, he said, is likely to spread the virus to 30% of others in the home.
“A few weeks ago,” Aragón added, “I would have sworn to you we could manage this.” Now that ICUs are filled, he is no longer so confident.
Barbara Ferrer, Los Angeles County’s public health director, showed the strain of her job during a Dec. 9 appearance. After matter-of-factly reciting that the death toll had exceeded 8,000 in L.A. County, she had to stop and swallow sobs. “Sorry,” she said.
Since then, an additional 800 L.A. County residents have died of COVID-19.
Dr. Grant Colfax, San Francisco’s public health director, has resorted to asking residents to think about the fact that their parents, grandparents or children may be denied a hospital bed or adequate care because of overwhelmed hospitals.
“Would you want that?” he asked last week.
But there are glimmers of hope.
Colfax said the rate of new virus cases in San Francisco slowed a bit last week. If people heed the painful lessons learned from Thanksgiving, the number of new cases may yet diminish, he said.
Ferrer said that “if all goes well,” she would expect to see a stabilization or even a decrease in the number of new daily cases by Christmas.
“I’ve spoken to a lot of people who say, you know, for the first time, they are taking it more seriously, they’re very worried about what’s happening in our hospitals, and that they’re making some significant changes,” she said.
Stay-at-home orders work in part because they effectively relay a message to the public about rising risks, said Dr. Robert Wachter, professor and chair of the Department of Medicine at UC San Francisco.
“It is impossible to prove that the new orders are doing something,” Wachter said, “but I think without them, it is highly likely that we would be even worse off.”
Times staff writer Howard Blume contributed to this report.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.

















