Monkeypox cases more than double in L.A. County. One region is hit particularly hard
- Share via
The number of cumulative monkeypox cases has more than doubled in Los Angeles County in the last two weeks as officials race to better track the virus and more widely vaccinate more vulnerable communities.
There have been 1,105 cumulative monkeypox cases reported countywide as of Friday, according to data from the Department of Public Health. As of this week, that total includes the region’s first cases in a jail and in a homeless shelter, according to health officer Dr. Muntu Davis. The median age of people with confirmed monkeypox cases in L.A. County is 35.
Nearly half the county’s cases for which geographic information is available have been reported in the health service planning area for the central part of the county, which includes West Hollywood, Hollywood, downtown Los Angeles, Eagle Rock, Highland Park, Echo Park, Silver Lake, Los Feliz and Boyle Heights. About 12% of the county’s residents live in this region.
About 15% of L.A. County’s monkeypox cases are in an area that includes the San Fernando and Santa Clarita valleys, county health data show. Roughly 22% of county residents live in that region.
The Antelope and San Gabriel valleys have reported the fewest cases.
As monkeypox cases across California and the U.S. continue to rise, experts address some of the concerns and questions swirling about virus, and what activities people should consider risky, or not.
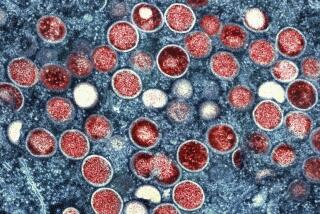
The disease — characterized by a rash and lesions that can look like pimples, bumps or blisters — primarily spreads through prolonged skin-to-skin contact with those lesions, which may be in hard-to-see places or mistaken for other skin issues. The lesions can appear first in the genital area and rectum before spreading to other parts of the body.
“Although cases are increasing in Los Angeles County, the risk of infection in the general population continues to remain very low,” Davis said during a briefing Thursday.
About 98% of cases for which there is gender identity information available are among males, county figures show. And 98% of cases for which sexual orientation is known are among people who identify as gay or bisexual, Davis said.
Although the disease can be quite painful, it is rarely fatal. Globally, there have been five deaths in the outbreak, none of which have been in the U.S.
“I want to reiterate that we continue to approach this outbreak with the utmost urgency to slow its spreading in California,” Dr. Tomás Aragón, California’s public health director and health officer, said Friday.
Monkeypox cases are rising exponentially, dimming hopes that officials can quickly gain control of the virus that has the potential to establish a lasting foothold.
Wastewater testing, which continues to prove useful in estimating the spread of the coronavirus, is also now being employed to track monkeypox.
In late June — about a month after the first California case was confirmed — monkeypox DNA was detected in wastewater in San Francisco, according to the WastewaterSCAN coalition, a group of scientists who have been testing sewage for the coronavirus since 2020.
“It helps understand how widespread this is,” said Stanford civil and environmental engineering professor Alexandria Boehm, one of the lead researchers on the WastewaterSCAN team.
The monkeypox virus also has been detected in L.A. County wastewater. Samples from the Joint Water Pollution Plant in Carson, which serves about 4 million residents and businesses in southern and eastern L.A. County, showed a small presence on July 31 and for three days during the first week in August, according to WastewaterSCAN data. The virus has not been detected there since, despite the rising case rates in the county.
By comparison, monkeypox DNA has been detected almost every day since June 27 at two wastewater facilities in San Francisco — and at much higher levels than in L.A. County.
Still, Boehm said that doesn’t mean there’s not more monkeypox in Los Angeles County; it’s just been difficult to detect among the massive sample size.
Because the L.A. County wastewater facility serves such a large number of people “you have to think about the sensitivity of detecting monkeypox relative to the incident rate in the population,” Boehm said. “Just because you don’t detect monkeypox, doesn’t mean there’s nobody [in that waste watershed] with monkeypox.”
Monkeypox DNA was recently detected in Los Angeles wastewater, as it has been for almost two months in San Francisco sewage.
It is not immediately clear whether the L.A. County Department of Public Health plans to expand monkeypox testing in wastewater. The county has been monitoring wastewater for the coronavirus for months, including at the Joint Water Pollution Plant, as well as at the Hyperion Water Reclamation Plant in Playa del Rey and facilities near Lancaster and Malibu.
“It will take some time to look and assess the correlations between the concentrations and the case counts. ... [But] we’re excited to be part of a larger group that’s figuring out how to best use the wastewater data,” L.A. County Public Health Director Barbara Ferrer said.
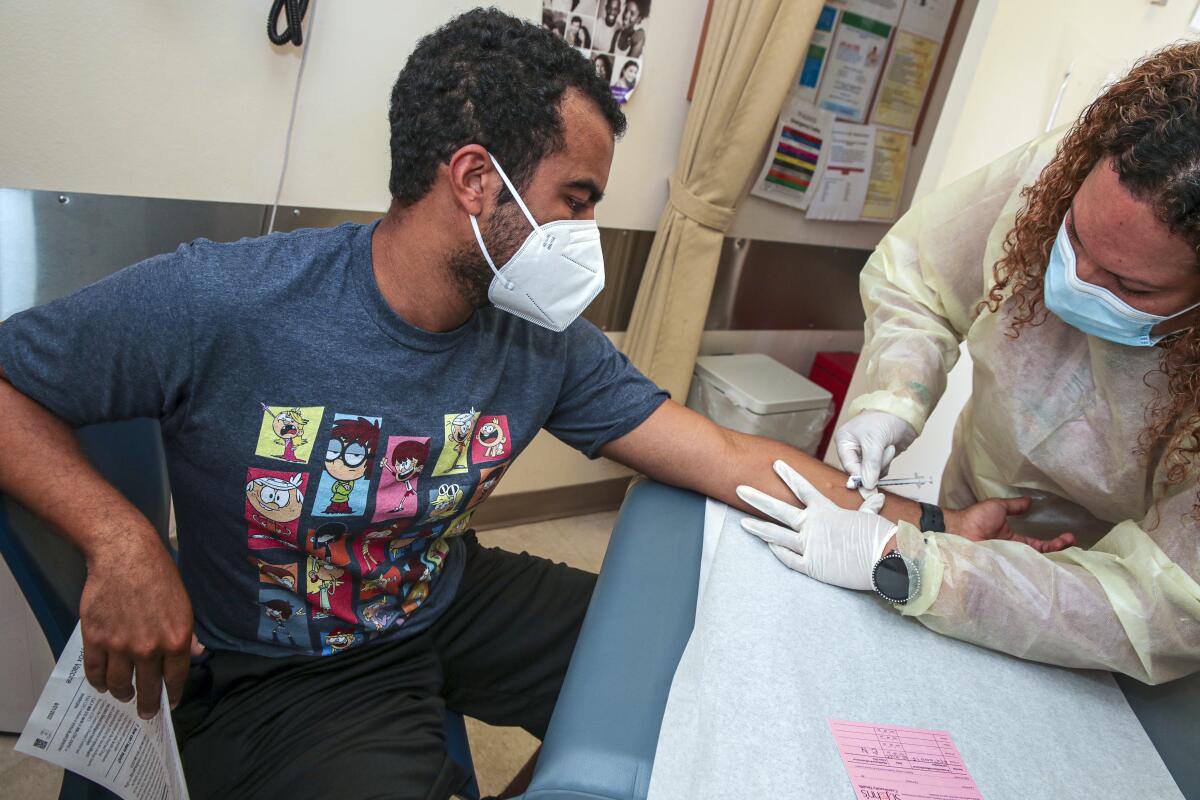
As of last week, L.A. County had received more than 43,000 doses of the Jynneos monkeypox vaccine. Nearly all — 91% — of those have already been administered, with the county offering second doses of the two-shot series for the first time this week. People are eligible for their second shot 28 days after their first dose and are considered fully vaccinated two weeks after their second dose.
Eligibility for the Jynneos shot also was expanded to children at high risk for the virus.
An additional 29,000 doses of the vaccine have just been received, Davis said Thursday. The latest vaccines will be used in the new method of administering doses intradermally — between layers of skin — instead of subcutaneously, in which the shot is injected in the fat beneath the skin. The new strategy allows each dose to now be one-fifth the volume of the originally sized doses, thus stretching the limited supplies.
People eligible for the monkeypox vaccine in L.A. County include gay or bisexual men and transgender people who have had multiple or anonymous sex partners in the last 14 days. Residents who are immunocompromised, including those with advanced or controlled HIV infection, are being prioritized for the immunization.
Prior data from Africa suggest the Jynneos vaccine is at least 85% effective in preventing monkeypox. Because the vaccine is not 100% effective, health officials still advise taking measures to lessen infection risk. But should infection still occur, “hopefully, it will make the infection less severe,” Davis said.
Aragón said the state has positioned close to 3,000 oral and 345 IV versions of Tpoxx treatments. Vaccines are being distributed in communities based on the number of cases reported by a county, he said.
How monkeypox spreads, how to get a vaccine and more: Your frequently asked questions about monkeypox, and answers from experts.
He noted that the trendline in cases will start to flatten or decrease when the virus “has trouble finding susceptible people to infect.” That could happen by people developing immunity through vaccination or prior infection, or if they “change their behavior and they’re not out there having as much contact, so that means there’s less opportunities for transmission to occur.”
“Those three things coming together is what’s going to drive the epidemic curve down,” Aragón said.
The California Department of Public Health this week released updated guidance recommending that those with a confirmed or suspected monkeypox case should isolate at home until either infection has been ruled out or their lesions are fully healed, a fresh layer of skin has formed and they’ve been free of other symptoms for at least 48 hours.
Residents can resume limited, lower-risk activities if they’ve been free of fever, respiratory symptoms or new lesions for at least 48 hours and any lesions that can’t be covered — like those on the face — are fully healed. In that instance, residents would need to bandage or cover any unhealed lesions, wear a well-fitting mask when around others; and avoid crowded settings, sharing towels or personal objects, and direct skin-to-skin contact.
People who have had monkeypox do not need the vaccine because they are immune, according to the county Department of Public Health. People who got the first dose of vaccine and were later infected generally don’t need the second dose; however, a second dose may be suggested by a healthcare provider.
County officials have begun to make vaccinations available to high-risk people in the county jail system and among homeless people.
Officials have long said the risk of monkeypox exposure is primarily through intimate skin-to-skin contact, and transmission of the virus has not been seen in this outbreak through surfaces at gyms or other public surfaces.
However, in 2018, there was a single documented case of monkeypox transmission in Britain in which a healthcare assistant was infected with monkeypox after changing “presumably contaminated bedding” without wearing a face mask or respirator. The worker had contact with the sheets during a time at which the patient had skin lesions but hadn’t yet been diagnosed with monkeypox and placed under isolation, according to medical journals.
At least 2 cases of monkeypox are confirmed in L.A. County children, but health officials say the risk for kids remains low, including in school.
Davis suggested that workers who are cleaning surfaces in settings that are touched frequently, such as gym equipment, or laundering bedding, towels and uniforms, take care to implement reasonable general-prevention practices that also protect against COVID-19 and other illnesses.
Workers should wear disposable gloves when cleaning, and workplaces should make handwashing facilities and hand sanitizer available for employees and customers, Davis said.
“We also encourage businesses where workers provide personal care services — such as massages or skin treatment — to consider posting signage asking customers or clients to delay services if they are experiencing symptoms, or if they have new or unexplained rashes, bumps, pustules, blisters or scabs that started as blisters,” he said.
Also recommended is “that workers visually inspect the area of skin that will be touched. And, of course, workers should not under any circumstances touch a rash,” Davis continued.
Residents can request the monkeypox vaccine through their regular healthcare provider or sign up online with the county Department of Public Health to request a vaccination. They also can call the health agency at (833) 540-0473, seven days a week between 8 a.m. and 8:30 p.m.
Times staff writer Melody Gutierrez contributed to this report.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.