COVID is still killing hundreds a day, even as society begins to move on

Roshan Kalghatgi was shocked when his 73-year-old mother tested positive for the coronavirus in July, nearly 2½ years into the pandemic.
“I thought it was a fluke,” the Redwood City resident said. “I made them do it again.”
His mother, Manisha, had eluded the virus at a Pennsylvania assisted living facility as COVID-19 devastated group facilities for the elderly. She had avoided infection again when she flew across the country to join Roshan and his family in San Mateo County, where she would tickle her 4-year-old grandson and faithfully follow his repeated requests to show him her belly button.
She had been vaccinated against COVID and received booster shots as well, Roshan said. By July, COVID wasn’t the top threat to Manisha on his mind: His mother had been struggling with kidney disease and Roshan fretted about how to keep her going to dialysis, which she had abandoned even as Roshan agonized about what it would mean for her health.

Manisha was “stubborn about the right things and also stubborn about the wrong things,” Roshan said ruefully, remembering how she had raised two children alone after the abrupt death of his father from a heart attack; and how she had moved repeatedly to find the best schools and services for Roshan, who became an engineer, and his sister Reena, who has an intellectual disability.
She died in August. To lose her now, Roshan said, “just seems so strange.”
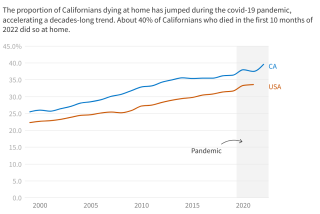
Americans have been urged to learn to live with the coronavirus, but this summer, hundreds were still dying from it each day. The death toll has fallen from the grim peaks of past surges, but has persisted in recent months, averaging more than 400 lives lost a day from June through August, according to data from the Johns Hopkins Coronavirus Resource Center.
At that rate, COVID still amounts to one of the biggest causes of death in the U.S., even as public officials herald the availability of vaccines and treatments. The coronavirus “no longer controls our lives,” President Biden declared this spring and again this summer. His COVID-19 coordinator has stated that most COVID deaths are now preventable.
Yet in Los Angeles County, more people died of COVID between May and July this year than during the same months last year. The virus claimed the lives of nearly 800 people in L.A. County in those months, compared with nearly 500 a year earlier. Elderly people bore the brunt of that increase, with a death rate that had tripled among people who had reached their 80th birthday.
“There’s no question in my mind that ageism has been an enabling aspect of our inadequate response to COVID,” said Dr. Michael Wasserman, a geriatrician and chair of the public policy committee for the California Assn. of Long Term Care Medicine.
Across California, roughly half of COVID deaths this summer were among people who had reached age 80 or older, and nearly one-third were between 65 and 79, a Times analysis of state data found.
Men remain more likely to die than women, according to L.A. County data. The toll of the pandemic has also continued to follow longstanding patterns of racial inequality: Black Californians had the highest rates of death from COVID across the state in recent months, a pattern that persisted in most age groups, The Times’ analysis found.
Advisories about enterovirus D68, or EV-D68, have been issued after the CDC noted more children were being hospitalized for severe respiratory illness.
But others were not spared, the figures show. Besides the stark toll on the elderly, hundreds of middle-aged and younger people also lost their lives to the virus in California in recent months, including four minors. Experts said that the rampant spread of the Omicron variant has driven up the number of deaths even as many others are surviving infection.
Right now, “the deaths have almost become an afterthought. We’re not really acknowledging what’s happening,” said Michael T. Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota. With hundreds still dying each day, “I just refuse to accept this as the norm. What are we doing wrong?”
*
Even last year, as vaccines became available, COVID continued to slash life expectancy in California, researchers found in a study published this summer in the Journal of the American Medical Assn. The worst hit were Black and Latino people in areas with low incomes.
Experts believe the heavier toll for Black and Latino patients has been tied to a host of factors, including crowded housing and face-to-face jobs that put them at higher risk of getting infected in the first place. And then there are longstanding inequities in who suffers from chronic illnesses such as diabetes, which leave people more vulnerable when the virus hits.
In Los Angeles County, the vast majority of people who died from COVID between May and July had at least one comorbidity, and nearly half had three or more, including hypertension, cardiovascular disease, obesity and other conditions. People in poorer neighborhoods have also been dying at higher rates than those in richer areas.
At Pomona Valley Hospital Medical Center, patients who have died of COVID in recent months have mostly been seniors, and “typically they have other comorbid illnesses” such as heart disease, said Dr. Rakesh Sinha, a pulmonary critical care specialist. Some have “long-term hypertension. Many of them have diabetes. And some of them are immunocompromised. They may have had cancer in the past. They could be on immunocompromising medications for rheumatoid arthritis or, at times, on steroids for their chronic illnesses.”
As COVID has persisted as a health threat, “it gets harder and harder for COVID to pick off the most vulnerable, because a lot of the most vulnerable have already perished,” said Andrew Noymer, associate professor of population health and disease prevention at UC Irvine. But as the virus endures, a new cohort of people are developing hypertension, asthma and other conditions, and “it can get its talons into a new generation.”
Some of the hardest hit have not gotten booster shots, Sinha said, and some have not been vaccinated at all against the coronavirus.
Federal data have shown that although vaccinated people have had breakthrough infections, they remain much less likely to die of COVID than unvaccinated people, especially if they had also received booster shots. As of early July, unvaccinated people 50 and older were more than a dozen times more likely to die of COVID than vaccinated people of the same ages who had two or more boosters.
But booster coverage has been spotty, even among the elderly, the bulk of whom got the initial vaccines, according to federal data. And fewer than 6% of immunocompromised people have been protected with Evusheld, a pair of shots that can armor them with antibodies that they do not generate from vaccination, CDC researchers have estimated.
And although their risk is much lower, vaccinated people have nonetheless been among those who have died from COVID. In California, 651 people who had received at least a primary series of vaccinations died of COVID in June and early July out of more than 28 million vaccinated people ages 5 and older, according to state data.
“The reality is that, nowadays, it’s not just unvaccinated people,” said Kristin Urquiza, cofounder of Marked by COVID, a nonprofit that has pushed for public recognition of pandemic deaths. “Especially for people who already have marginalized health and are immunocompromised or disabled.”
After his mother tested positive for the coronavirus, Roshan Kalghatgi was unable to see her for a week. “At some point I said, ‘Screw it — I’m going in there.’”
He suited up in protective gear to sit at her bedside as she was in hospice care. When she died, he lamented the fact that they had not been able to spend her last days doing things she loved: listening to Hindu devotional music, snacking on idli with chutney or indulging in McDonald’s fries, playing with her grandson, or just talking.
“We just couldn’t have those last moments,” he said. She had been preparing to die, but “her wishes did not include COVID-19,” he added.

Many of the high-risk patients that Dr. Thomas Yadegar takes care of “were able to protect themselves, and one way or another they were able to evade this virus — up until the last few months, when it’s been impossible because it’s so much more contagious and has been so prevalent,” said Yadegar, medical director of the intensive care unit at Providence Cedars-Sinai Tarzana Medical Center.
He lamented that other people had become “complacent” and unwilling to take simple steps such as wearing a mask indoors to protect those at highest risk.
“We’ve sacrificed the lives of our most vulnerable for our own convenience,” Yadegar said. “The elderly, the immunocompromised, and the unvaccinated or under-vaccinated — they are the ones that account for the vast majority of deaths due to COVID-19.” As hundreds perish daily, “thousands more are left behind, tormented by the loss.”
*

Days after Paul Alweyn Redd Jr. got COVID, his sister texted him to tell him not to worry about a family errand — to just focus on taking care of himself — and to call back and let her know how he was doing.
“He never did call me back,” Alvina Williams said, growing tearful. “And he always called me back.”
Redd, 65, had spent decades in prison after being convicted of a murder he said he didn’t commit. He had also grappled with cancer and started undergoing chemotherapy while incarcerated. But he had made it through those ordeals — and when he was released, after a judge reduced his conviction to manslaughter, “it was like he had never left,” Williams said.
The Oakland resident showed up at every birthday party and family barbecue, crisply dressed in a matching outfit, cracking jokes to make his younger sister laugh. “He always wanted to take care of family,” Williams said. “That was his main mission — to come out and take care of those that had taken care of him.”
Redd also tried to take care of those he had left behind. His nephew U-Gene Jackson remembered that when he got out of prison, after celebrating with a steak, he quickly started unloading plastic tubs full of paperwork on the kitchen table, trying to decide who he needed to call first.
“He felt like, ‘I’ve got to get these guys out of here,’ ” Jackson said.
He went to work as a legal assistant, trying to help others still locked up. He logged onto Zoom calls with lawyers and spoke at rallies.
No matter what he was doing, though, Williams said Redd would pick up the phone when she called and tell her he would call her back. Even if he were on stage, she said, “he would answer and say, ‘Sis, I’m giving a speech, I’ll call you back.’ ”
But this time, he never called. Redd had told her, when she had initially phoned to ask if he could pick up their sister from the airport, that he wasn’t sure if he could make it. “Sis, this COVID ain’t no joke,” Williams remembers him saying.
She knew he had already been grappling with the cancer that had come back, this time hitting his lungs. Jackson said Redd had been vaccinated and received booster shots, but “I think he was much sicker than what he led us to believe,” even before he got COVID.
Osterholm, the University of Minnesota expert, said that for people with other medical vulnerabilities, COVID can be like a lit match thrown into dry brush. “It doesn’t cause the high temperatures, or the winds, or the low humidity” that spell disaster, he said. “But nothing happens until you throw that SARS-CoV-2 virus into the mix.”
Redd died on June 19 at home at Canticle Farm, a social-justice-oriented community built around a garden in the Fruitvale neighborhood. At his funeral, mourners wore red — his surname and his favorite color — and released doves.

Depression has weighed on Williams in the months since his death. Williams cannot bear to look at his obituary. She cannot bring herself to pick up his book of poems, including one addressed to her, “my pride and joy.”
“As a society, we are not really fully processing what it means to lose people in the way we have,” said Vickie M. Mays, a UCLA professor in psychology and health policy and management.
When people talk about death, they often think about the individual and their immediate circle, but losing elders can also mean the disappearance of languages or the disruption of communities that relied on them as caregivers, she said. “The loss of one person reverberates out. You’re looking at touching many lives.”
Jackson said in a family that had been flung apart by distance and tragedy, Redd “was like the glue.” Even while he was in prison, he had used letters to introduce Jackson to cousins he never knew he had. Now, “I don’t think it’ll be the same,” Jackson said. “Everybody will kind of go back to their clamshells.”
*

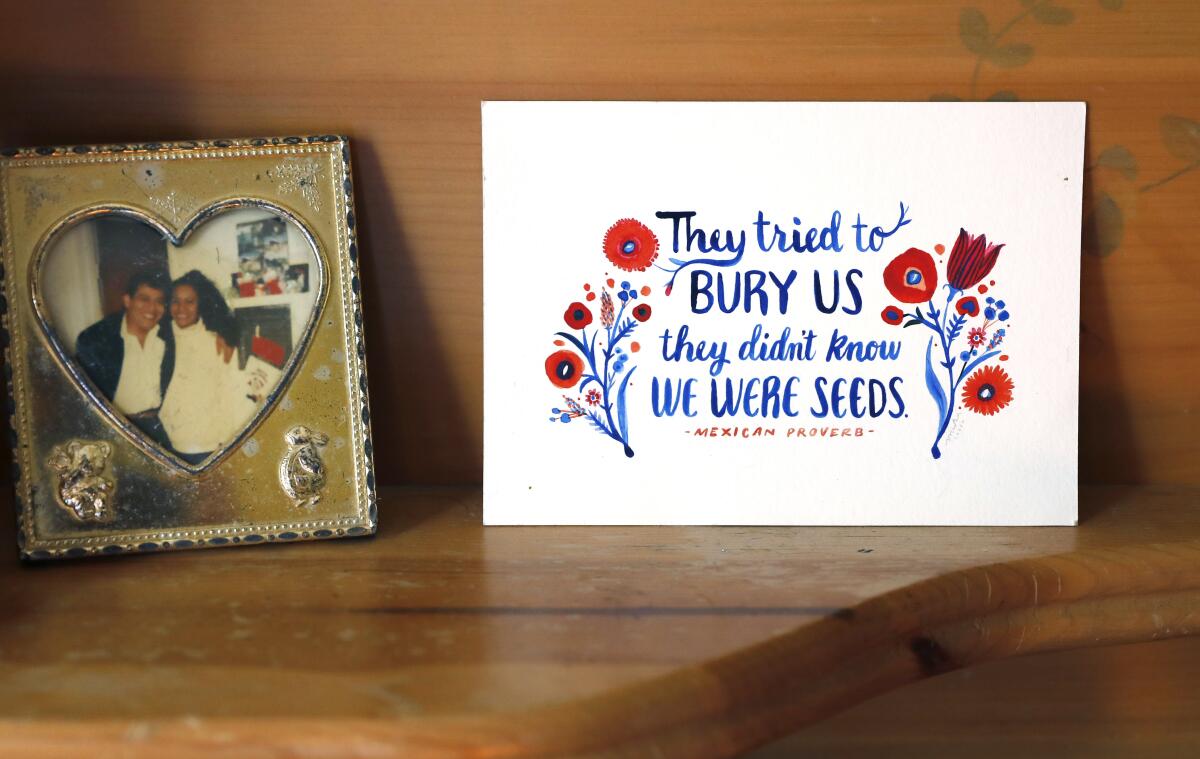
Erick Morales remembers his mother asking him to translate the English saying off the Christmas card that her bosses had given her. “It was something like, ‘They tried to bury us but they didn’t know that we were seeds,’” he remembered. “She really liked that. I know it’s like a card, but that stuck with her for a really long time.”
Alejandra Gutiérrez, 59, had uprooted herself to make a life in a new country, working hard as a housekeeper to provide for her family in Los Angeles. She had lost the father of her children to cancer and become the sole parent to Erick and his sister Alejandra when they were just 5 and 4. Yet she had emerged from her grief with a buoyant faith.
Her daughter Alejandra remembers that she loved to bring people hope, gathering groups of Pentecostal churchgoers in her home to share the word of God. As a mother, “she always met me where I was at,” Alejandra Morales-Gutiérrez said. “She never made me feel like I was in the wrong for feeling what I was feeling.”
Even when she fell ill, Gutiérrez was generous with her daughter about her frustration and sadness, her daughter remembered. She was diagnosed with ovarian cancer during the first winter that COVID-19 was battering hospitals. Her son and daughter avoided going out much, trying to protect her from the virus as she underwent chemotherapy.
The new Omicron COVID-19 vaccine is useful but shouldn’t skew our expectations of the pandemic’s future.
The cancer metastasized to her brain in January. She endured radiation, then surgery on her gall bladder. In late May, her children checked her oxygen levels after seeing her struggle with breathing. Doctors suggested a COVID test, which came back positive. They shuttled her back to one hospital, then headed to another when no bed could be found for her.
She died at home, while in hospice care. In her last days, she could not speak. Morales-Gutiérrez painted her nails and curled up next to her to watch a Spiderman movie. She played worship music that her mother loved. The family gathered around her and prayed and told her that it was OK if she no longer wanted to fight.

After her death in June, her children discovered that she had bought insurance to help cover some burial expenses and picked out her casket ahead of time, trying to make things easier on them. “It just goes to show how caring she was as a mom,” Morales-Gutiérrez said.
They had tried hard to protect her too, wearing masks inside the house while she endured chemo and radiation, turning down invitations to go out with friends to avoid COVID. They wonder: Did they somehow infect her anyway? Or did she get it at the hospital? She was vaccinated and had gotten one booster shot, but not a second. Would it have made any difference?
What nags at Dr. Eric Topol are all the things we do not know about the hundreds of people dying daily of COVID across the country. He wonders: “Did they get Paxlovid? Did they get bebtelovimab?” Medications can help fight the virus, but “what if people just didn’t get the therapies that they need? How many of these deaths were avoidable?”
After a death, doctors usually hash out whether it was avoidable. Now it’s happening hundreds of times a day, “and there’s no interest in doing a postmortem of the problem,” said Topol, director of the Scripps Research Translational Institute in La Jolla.
Instead, the impulse is often to wave it away. When someone loses a loved one to COVID, “often the first thing that’s asked of you is either, ‘Were they vaccinated?’ or ‘Did they have a preexisting condition?’” said Urquiza of Marked by COVID. “I think people are asking that because they want to reaffirm their own sense of safety. ‘Oh, Kristin’s dad died because he had x, y or z — I don’t.’”
Morales said that people tend to assume that cancer alone took his mother. When he told a friend that she ultimately died after getting COVID, the friend was surprised.
“‘Really? COVID? How did that happen?’” the friend asked Morales. “‘People aren’t dying of COVID anymore.’”
Times staff writer Sean Greene contributed to this report.
More to Read
Updates
4:44 p.m. Sept. 22, 2022: This article was updated with recent state data showing that in California, 651 people who had received at least a primary series of vaccinations died of COVID in June and early July, out of more than 28 million vaccinated people ages 5 and older.
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.