COVID-19 is on the rise this summer. What to know, how to stay safe
It is not your imagination — more people this summer are getting COVID-19.
Officials are monitoring a recent uptick in coronavirus transmission, but say it is too early to know how this will go. Hospitalizations and deaths are still very low compared with the peaks of the last three years.
Here is what you need to know:
What do we know about the latest summer uptick?
National: The U.S. recorded a 10% increase in new COVID-19 hospital admissions for the week that ended July 15 compared with the previous seven-day period. Still, hospitalizations remain near a record low for the pandemic. Hospitalizations are rising fastest in the South, Great Plains and Rocky Mountain states. California, so far, has fared better.
Summer has brought an uptick in coronavirus transmission, but experts say it is still too early to tell whether this represents a significant health concern.
California: Coronavirus levels in Los Angeles County wastewater have been trending upward. And the statewide test positivity rate hit 7.6% for the week that ended Monday, up from 4.1% a month earlier. The number of coronavirus test results reported to the California Department of Public Health has also doubled over the last month, a possible indication that more people are getting sick — or are at least concerned they have been exposed to the virus. COVID-19 hospitalizations in California, while still near record lows, are no longer decreasing.
Why do experts think cases are going up?
Travel: Summer travel has roared back from pandemic-era lows. The Transportation Security Administration recently said that, nationally, June 30 was the busiest day ever for the agency’s operations, exceeding the previous record set on the Sunday after Thanksgiving in 2019.
Behavior: Vacations and conferences are back in earnest. And most activities now taking place entirely or largely without masks — boosting the chances for infection, experts say.
Timing: Most people got their last COVID-19 booster shot months ago, if not longer. And given that the most recent coronavirus uptick occurred last winter, many haven’t been exposed to significant circulation of the virus for quite some time.
New study suggests that people with a specific version of a particular gene who got COVID were far more likely to experience an asymptomatic infection.
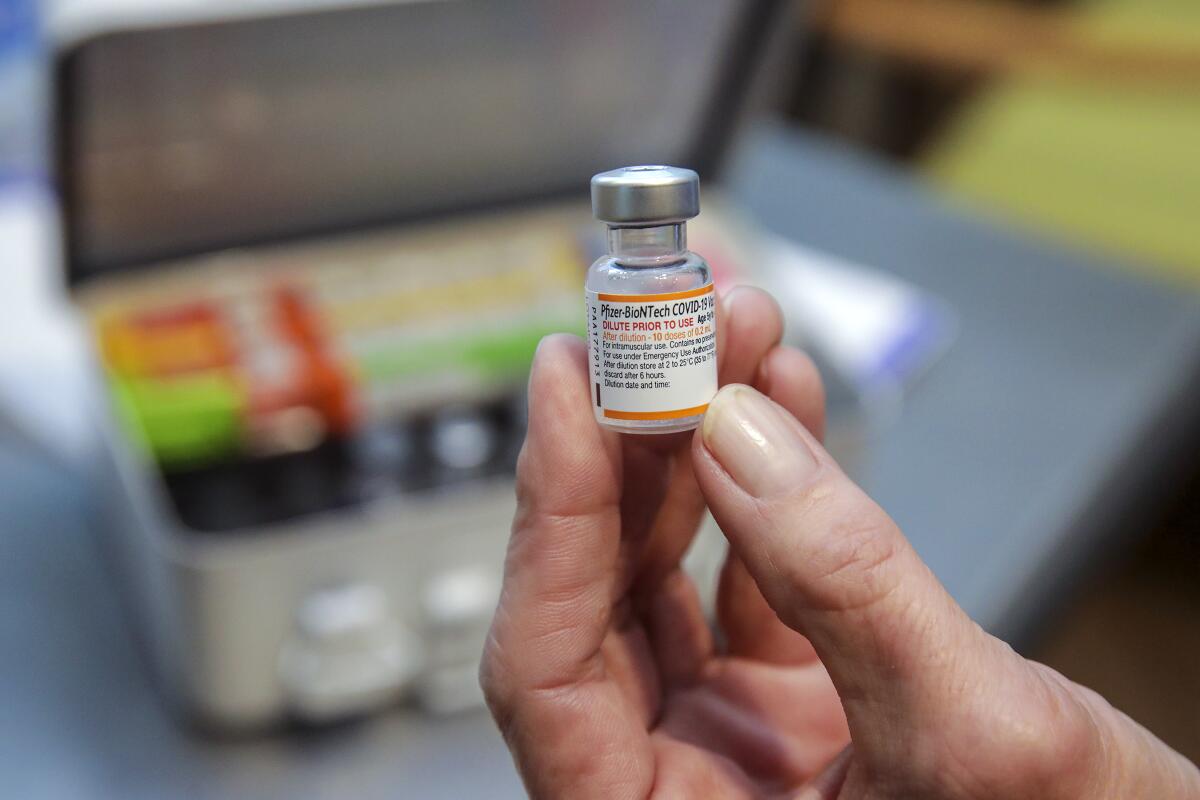
What about vaccines?
Vaccines are available for COVID-19 and the flu — and officials say rolling up your sleeve is a potent way to ward off severe illness.
The updated COVID-19 booster shot became available in September, but most people haven’t gotten it. Statewide, 21% of residents are considered to be up-to-date on their COVID-19 vaccination, according to the California Department of Public Health. By contrast, 73% of Californians have received their primary — generally two-dose — vaccination series.
The bivalent booster is formulated to protect not only against the original coronavirus strain, but also the Omicron subvariants that dominated the nation throughout much of the year — namely BA.5.
Some experts and officials have hypothesized that the cadence of COVID vaccinations will eventually mirror that of flu: one shot updated and administered annually.
The plan for September is to roll out a reformulated COVID-19 vaccine designed against the Omicron subvariant XBB.1.5 to replace last September’s version, which was targeted against a different strain, BA.5.
The CDC now estimates XBB sublineages comprise nearly 99% of circulating coronavirus in the U.S., displacing the BA.5 subvariant that dominated the nation for much of last year.
What about Paxlovid?
Now that Paxlovid, an anti-COVID oral drug that can be taken after infection, has been fully approved by the U.S. Food and Drug Administration, higher-risk people can talk to their healthcare providers about getting Paxlovid before, say, an overseas trip if they think it’ll be hard to obtain the drug later. That would enable people to take the pills quickly should they test positive for the coronavirus.
It can be helpful to have the Paxlovid conversation before becoming sick with COVID-19. That way, patients can talk with their regular healthcare providers about the possibility of interactions with other drugs they are taking.
The FDA says Paxlovid significantly reduces the percentage of people with COVID-related hospitalization or death from any cause.
Test positivity has ticked up in L.A. County in recent weeks, though we’re still well below peak COVID levels. If you get COVID now, here’s how to treat it, how long to isolate, how to get Paxlovid, and more information on getting healthy.
What are some other safety tips?
- It’s a bummer to cancel events, especially after all the interruptions of the last few years, but even a tickle in the throat or feeling under the weather should be cause enough to stay home until you feel better.
- There’s a reduced risk of viral transmission outdoors. At events and gatherings, it’s better to offer beverages and food outside, if possible. Improving ventilation by opening doors and windows, or using an air purifier, can also help.
- Officials say avoiding sick people and getting tested if you have COVID symptoms remain prudent steps to avoid infection. Keeping a mask handy so you can wear it if needed — for instance, if you’re unlucky enough to sit on a plane next to coughing people spraying droplets in your face — would also be a good idea.
And, as always, experts emphasize the benefits of practicing good health habits — getting plenty of sleep, being physically active, eating nutritious food, drinking plenty of fluids and managing your stress.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.















