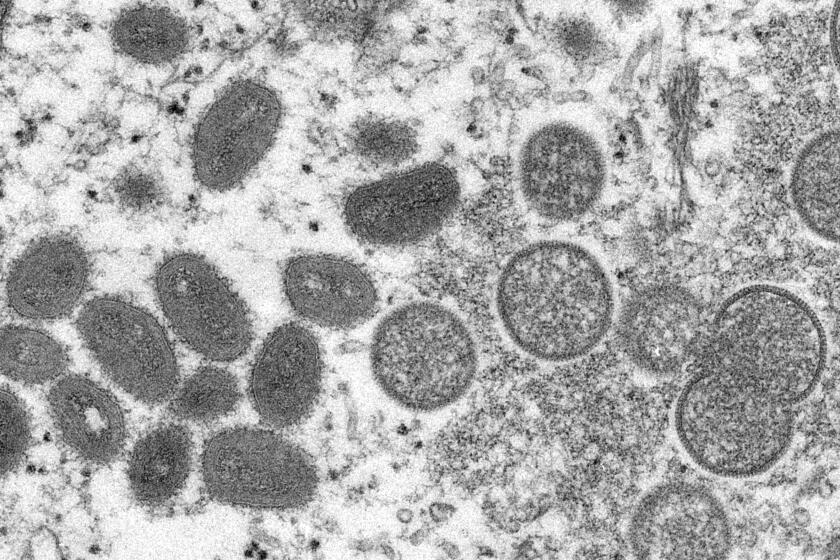
Can the spread of monkeypox be stopped?

LONDON — Since May, nearly 90 countries have reported monkeypox, totaling more than 31,000 cases.
The World Health Organization classified the escalating outbreak of the once-rare disease as a global emergency in July; the U.S. declared it a national public health emergency last week.
Outside of Africa, 98% of cases are in men who have sex with men. With only a limited supply of vaccines, authorities are racing to stop monkeypox before it becomes entrenched as a new disease.
Can monkeypox be contained?
Theoretically, yes. The virus does not spread easily and there is a vaccine. But there are only about 16 million doses available now, and only one company makes the shot.
Except for Africa, there is no sign of sustained monkeypox transmission beyond men who have sex with men, meaning that stopping spread among that group could effectively end the outbreak. Last week, British scientists said there were “early signs” the monkeypox cases in the U.K. — which once had the world’s biggest outbreak outside Africa — had peaked.
Monkeypox cases are rising exponentially, dimming hopes that officials can quickly gain control of the virus that has the potential to establish a lasting foothold.
Is this another pandemic?
No. A pandemic means that a disease outbreak has spread to the entire world. Monkeypox does not transmit as quickly as the coronavirus, and stopping it will not require dramatic interventions like the COVID-19 lockdowns.
To the public, the monkeypox outbreak has echoes of the early days of the COVID-19 pandemic. But scientists say it’s not the same at all.
WHO Director-General Tedros Adhanom Ghebreyesus said he declared monkeypox an emergency in part to prompt countries to take the epidemic seriously, saying there is still an opportunity to contain the disease before it becomes a global problem.
How does it spread?
Monkeypox spread typically requires skin-to-skin or skin-to-mouth contact with an infected patient’s lesions. People can also be infected through contact with the clothing or bedsheets of someone who has monkeypox lesions.
It also can be spread through contact with respiratory droplets, but scientists are still trying to figure out how often that happens. British health officials say they haven’t confirmed any instances of airborne transmission.
Who is getting infected?
A large percentage of cases have been in gay and bisexual men. The initial outbreaks in Europe and North America were likely triggered by sex at two raves in Spain and Belgium.
According to the U.S. Centers for Disease Control and Prevention, 99% of monkeypox cases in the U.S. involved men. Of those, 94% reported sexual contact with other men in the three weeks before they developed symptoms.
Although the monkeypox virus can affect anyone, some gay and bisexual men are worried about being once again branded as carriers of an exotic disease.
Still, anyone can catch the virus if they are in close contact with an infected person or fabrics that touched an infected person.
Who is getting vaccinated?
With supplies limited, health officials are not recommending mass vaccination. They are suggesting the shots for health workers, people who have been in close contact with an infected person, and men at high risk of catching monkeypox.
Officials are also trying to stretch supplies of the vaccine, Jynneos. It requires two doses, but many places are giving only one dose.
Who is eligible to get the monkeypox vaccination in Los Angeles right now? And how to do you get one? Here’s what to know.
U.S. health officials on Tuesday authorized a new strategy that would allow health professionals to vaccinate up to five people — instead of one — with each vial. The approach uses just a fraction of the typical amount of vaccine and administers it with an injection just under the skin rather than into deeper tissue. Recipients would still get two shots a month apart.
What else can I do to lower my risk?
Tedros recommended that men at risk of catching monkeypox consider making “safe choices” and reducing their sexual partners “for the moment.”
Britain’s Health Security Agency has advised people to check themselves for monkeypox lesions before they have sex or go to a social event, noting that most of the country’s cases are believed to have originated at festivals, saunas and other venues where sex has taken place. Anyone with monkeypox lesions should isolate until completely healed, which can take up to three weeks.
Gay and bisexual men, transgender people and others worried about monkeypox are strategizing to protect themselves as they wait for vaccinations.
What’s the connection to Africa?
Monkeypox has been endemic for decades in parts of central and west Africa, where people have mostly been sickened after contact with infected wild animals like rodents and squirrels. The acting director of Africa’s top public health agency said last week that sex among gay and bisexual men was “not relevant” to the continent’s outbreak, with about 40% of cases among women.
Scientists think the monkeypox outbreaks in Europe and North America originated in Africa long before the disease started spreading. Viral samples from cases in Europe show dozens of mutations, suggesting the initial virus was silently spreading for months or years before the current epidemics were detected.
The version of monkeypox spreading in Europe and North America has a lower fatality rate than the one circulating in Africa. Countries that didn’t see many monkeypox cases before this outbreak have reported a handful of deaths, while Africa has had at least 100 suspected deaths this year.
Who is at higher risk for serious illness?
Most people infected with monkeypox recover without treatment, but it can cause more severe symptoms like brain inflammation and in rare cases, death.
Monkeypox can be serious in children, pregnant women and people with underlying health conditions, like cancer, tuberculosis or HIV. In the U.S., the CDC says about 40% of people with monkeypox also have HIV.
For many Californians suffering from monkeypox, getting Tpoxx has not been simple. The smallpox drug has not yet been approved by the FDA to treat monkeypox.
The longer the current outbreaks continue, the greater the chances the virus could spread in other communities, similar to how HIV was first spotted in gay men before becoming established more widely.
“There is some crossover between the sexual networks of gay and bisexual men and networks of heterosexual people with high sexual activity, so it is possible we could see monkeypox more widely,” said Dr. Paul Hunter, a professor of medicine at Britain’s University of East Anglia. “If that happens, we may have a much bigger problem.”
AP writers Mike Stobbe in New York and Matthew Perrone in Washington contributed to this report.